| |
|
|
INTRODUCTION
Typical clinical symptoms in Transient Ischemic Attack (TIA) last
less than one hour and there is no neuroradiology evidence of
cerebral infarction. Usually, it is caused by arterial stenosis.
However, sometimes other pathological processes can cause the same
phenomenon [1].
CASE REPORT
A 51-year-old male with a history of hypertension, tobacco
smoking and ten-year professional exposure to radiation was admitted
at the Admission Unit of the Emergency Centre with symptoms of
recurrent right-sided weakness. The symptoms repeated several times
in the previous few days, appearing only during physical activity
and reduced at rest, lasting up to 15 minutes. There was no
headache, vomiting, dizziness, disturbances of vision or speech.
Family history was negative for cerebrovascular, endocrine and
malignant diseases.
On admission the patient had no neurological deficite (NIHSS 1, mRS
0, ABCD2 scores 2). Physical examination was normal, save for oval,
painless, immobile tumour mass, soft in consistency at the left side
of the neck, near the sternocleidomastoid muscle (SCM),
approximately 5cm in diameter.
The thyroid gland was not palpable in its normal position.
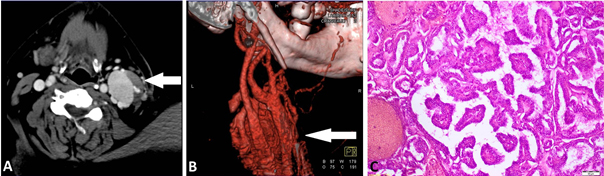
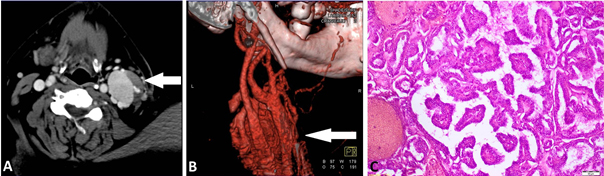
A contrast CT of the neck and CT angiography verified well-vascularized
tumour mass of the left side, size 4x3x4cm, located behind the SCM
(Figure 1A).
The tumour was fed by a branch of the external carotid artery
(Figure 1B). The thyroid gland was normal except for a small
calcification in the left lobe and completely isolated from the left
cervical mass. CT angiography excluded stenosis of carotid and
vertebral arteries which would require vascular surgical treatment.
However, a treatment with 100 mg aspirin per day was started.
A first non-contrast head computed tomography (CT) scan, as well as
the control one, 24 hour later, were normal. Carotid and vertebral
duplex ultrasound, as well as transcranial Doppler of intracranial
arteries, revealed normal findings. Basic metabolic panel and cell
blood count were unremarkable, except hypercholesterolemia. Thyroid
function test results were also normal, he was clinically euthyroid.
Electrocardiography monitoring and chest X-ray were normal.
After ten days, total neck tumour resection was done.
Histopathological analysis revealed metastasis of papillary thyroid
carcinoma (PTC) (Figure 1C). After three months, total thyroidectomy
was done and the patient received radioiodine therapy treatment
(131I). The definitive histopathological diagnosis was PTC. At
one-year follow-up, the patient was on substitution thyroid hormone
and antiplatelet therapy, without repeated episodes of neurological
symptoms.
Figure 1: A) CT of the neck shows cervical lateral
tumour mass on the left side.
Figure 1: B) CT angiography shows well-vascularised cervical tumour
mass with branches
of left external carotid artery.
Figure 1: C) Histopathological analysis revealed papillary thyroid
carcinoma with highly dilated
and numerous blood vessels. (HEx 40).
DISCUSSION
From the beginning, we were skeptical that the typical vascular
causes were bases of recurrent TIA in this case.
Brain CT and neuroultrasonography did not show cerebral infarction
or carotid artery disease. Blood supply of the left cervical mass
was found to be from the arteries "feeders" of the External Carotid
Artery (probably Artery Thyroid Superior) with drainage in the
Internal Jugular vein (IJV), but carotid angiography ruled out the
existence of arteriovenous malformation. After that, we suspected
ectopic thyroid tissue, but differentiation between a ectopic
thyroid carcinoma and a metastatic thyroid carcinoma can be very
difficult. According to the literature data, ectopic thyroid
carcinoma should be considered when there is separate blood supply
of the ectopic gland from extra-cervical vessels, no personal
history of malignancy, and normal or absent orthotropic thyroid with
no history of surgery [2,3].
In addition, total thyroidectomy and histopathological findings of
the thyroid gland still revealed primary papillary thyroid carcinoma
(PTC).
The most common of all thyroid carcinoma is PTC with genetic factors
and radiation exposure as risk factors. It usually has lymphatic
dissemination in regional lymph nodes (90%), while less common is
the hematogenous dissemination (2-5%) [4].
On the other hand, distinguishing transient ischemic attack (TIA)
from nonischemic causes is difficult in the ER [5].
Up to 60% of patients referred to a TIA clinically do not have a
final diagnosis of TIA [6]. In addition to cardiovascular diseases,
various neoplasms of neck or head can also cause symptoms of the TIA,
by mechanism of compression, infiltration, or vascular steal
phenomenon [7].
Although it could just be a coincidence, hypervascularized
metastasis of PTC neck tumour in this case could cause TIA symptoms
by mechanism of carotid compression or steal phenomenon in physical
activity. After the surgical resection of the tumour, the
neurological symptoms did not repeat.
To our knowledge, we have described a rare and perhaps the first
case of such a large and well-vascularized metastatic thyroid
carcinoma causing TIA.
In conclusion, with TIA in ER, beside usual causes of TIA, always
keep on mind other, nonvascular diseases. So, you can expect
unexpected!
REFERENCES
- Kawahara I, Nakamoto M, Matsuo Y, Tokunaga Y. Subclavian
steal phenomenon associated with hypervascular thyroid tumour.
No Shinkei Geka. 2010;38(5):473-6.
- Noussios G, Anagnostis P, Goulis DG, Lappas D, Natsis K.
Ectopic thyroid tissue: anatomical, clinical, and surgical
implications of a rare entity. Eur J Endocrinol.
2011;165(3):375-82.
- Klubo-Gwiezdzinska J, Manes RP, Chia SH, Burman KD,
Stathatos NA, Deeb ZE et al. Clinical review: Ectopic cervical
thyroid carcinoma--review of the literature with illustrative
case series. J Clin Endocrinol Metab. 2011;96(9):2684-91
- Manganaris C, Wittlin S, Xu H, Gurell M, Sime P, Kottmann
RM. Metastatic papillary thyroid carcinoma and severe airflow
obstruction. Chest. 2010;138(3):738-42.
- Prabhakaran S, Silver AJ, Warrior L, McClenathan B, Lee VH.
Misdiagnosis of transient ischemic attacks in the emergency
room. Cerebrovasc Dis 2008;26:630–5.
- Nadarajan V, Perry RJ, Johnson J, Werring DJ. Transient
ischaemic attacks: mimics and chameleons. Pract Neurol
2014;14:23-31.
- Braakman HM, Knippenberg SA, de Bondt BJ, Lodder J. An
unusual cause of transient neurologic deficits: compression of
the carotid artery by a thyroid cystic nodule. J Stroke
Cerebrovasc Dis 2010;19:73-4.
|
|
|
|