|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
Page 114 |
||||||||||||||||||||||||||||||||||||
|
Case report Paraneoplastic syndrome as a possible cause of pulmonary thromboembolism in a female patient with nephrotic syndromeJasmina Mrgud (1,) Ana Jevrić (2), Vlastimir Vlatković (3),
Branislav Gašić (3) |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | SUMMARY: A
59-year-old female patient was admitted to the hospital due to
suffocation, lower leg swelling, and general weakness. She had been
treated previously with immunosuppressive therapy for several years
because of focal segmental glomerulosclerosis with nephrotic
syndrome. The expected therapeutic response was not accomplished.
Upon admission, the following were determined in the laboratory:
hypoalbuminemia, hyperlipidemia and nephrotic range proteinuria.
X-ray of the lungs showed bilateral pleural effusion, because of
which a pleural puncture was performed and which drained 800 mL of
fluid. Tumor markers test, breast echosonography and mammography
were performed, along with bone scintigraphy, which was done upon
the recommendation of an oncologist. Mammography described
microcalcifications bilaterally while bone scintigraphy showed
pathological accumulation of radiopharmaceuticals in the V thoracic
vertebra and sternum corpus, and III and IV ribs on the left. On the
fifth day of hospitalization, there was a deterioration of patient’s
general condition with hypotension, tachycardia and angina, as well
as an increase in D-dimer. On the ECG sinus rhythm, f 80 / min, low
voltage in standard and unipolar leads. Upon the recommendation of a
cardiologist, CT was performed according to the program for
pulmonary thromboembolism (PTE), which showed submassive PTE. Low
molecular weight heparin therapy was used, along with oxygen therapy
with dopaminergics, bronchodilators, human albumin and plasma
infusions, statins and transient treatment of hypervolemia by means
of hemodialysis. The patient was hospitalized for 61 days due to
multiorgan dysfunction. Breast magnetic resonance imaging was not
performed due to the poor general condition of the patient. Most
likely it was breast cancer with secondary deposits, which was
recognized late. PTE, as a probable consequence of paraneoplastic
nephrotic syndrome, was diagnosed and treated in a timely manner.
Key words: nephrotic syndrome; pulmonary thromboembolism; paraneoplastic syndrome |
|||||||||||||||||||||||||||||||||||
INTRODUCTIONPulmonary thromboembolism is a vascular disease that occurs as a complication of venous thrombosis and a thrombus breaking loose and reaching the lungs through circulation. The clinical picture also depends on the degree of occlusion and the number of affected pulmonary arteries (massiveness of the embolism). Annual frequency is 2-3 / 1000 inhabitants. The most common embolizations are proximal DVT 40%, VCS - 10-20%, distal DVT - 20-30%, upper extremities (CVC). Risk factors: trauma, orthopedic surgery (particularly hip and knee), major abdominal, thoracic, gynecological surgeries, vein surgery, cardiovascular diseases accompanied by cardiac decompensation and arrhythmias, septic conditions, long-term immobilization, childbirth, autoimmune diseases, as well as malignant diseases (pancreatic, breast, prostate and bronchus cancer). CASE REPORTMaterial used from the patient's medical history, medical data from the hospital information system KIS-UCC of Republika Srpska, patient’s letter of discharge from UCC of Republika Srpska. Results: The patient had a positive family history of
malignant diseases and a significant weight loss. Objectively of
cachectic appearance. Cor: Heart action rhythmic, fast, tones
quieter, no noise, TA 120 / 70mmHg. Pulmo: Ausculatory over the
lungs bilaterally diminished respiratory murmur. DE: Mutual
pretibial edema.
We conclude that the patient had thrombocytosis, grade III renal
insufficiency, normal mineral status, hypoproteinemia and
hyperlipidemia, nephrotic range proteinuria, metabolic alkalosis,
and elevated tumor markers for the breast and genital tract.
Gynaecology ultrasound findings were normal. On the fifth day of
hospitalization, the patient's clinical condition sharply
deteriorated. as problems, she reported suffocation, chest tightness
and dry cough. Objectively dyspnoeic at rest with central cyanosis
present, tachycardic heartbeat, quieter tones, no murmur, TA 80 /
60mmHg. ECG showed sinus rhythm, f 80 / min, low voltage in standard
and unipolar leads. Oxygen therapy was administered, Dobutamine 5mcg
/ kg / min (250mg Dobutamine in 250mL 0.9% NaCl), Clexane 0.6 ml 1x1
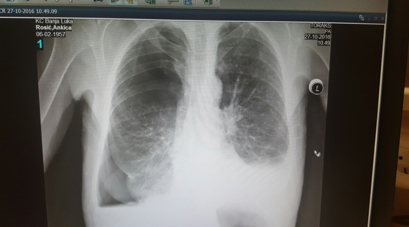
s.c; blood was taken for D dimer and cardiospecific enzymes. Figure 1. Chest X-ray (X-ray of the heart and
lungs) shows bilateral pleural effusion up to V rib as well as
encapsulated effusion in the projection of the lower lung area to
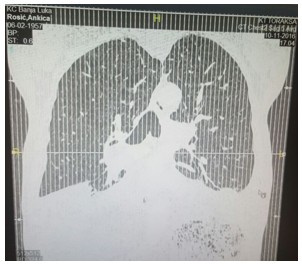
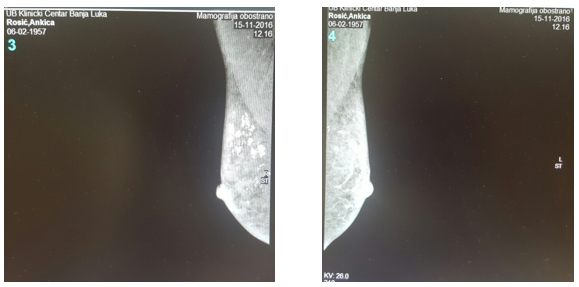
the right Computed tomography of the thorax (CT) according to the PTE program showed submassive thromboembolism of the right pulmonary artery (Figure 2). The defect in the lumen is differentiated - thromboembolism of the branch of the right pulmonary artery for the upper lung lobus with extension into segmental branches for the anterior segment as well as incomplete thrombosis of the intermediate branch of the right pulmonary artery. Pulmonary artery tree width 23mm, right pulmonary artery 21mm, left pulmonary artery 18mm. There is no consolidation or infiltration in the parenchyma shown. Posterobasal pleural effusion right about 5 cm wide, left up to 6 cm with consequent compressive atelectasis of the basal segments of the lower lung lobes. Figure 2. Chest CT according to the PTE protocol: Figures 3. and 4. Native mammography of both
breasts and the axillary region: Bilaterally prepectoral and more
pronounced in the right breast, multiple intraductal segmental
calcifications are observed, completely filling the ducts. Among
these amorphous calcifications, multiple individual
microcalcifications of suspected malignant characteristics are
observed DISCUSSION:Malignant tumors affect the body locally: by their mass, by infiltrative growth, by destruction of local tissue, by compression, through necrosis, bleeding, secondary infections. By systemically secreting hormones and other substances, they affect distant organs and systems or consume building material and energy. Paraneoplastic syndrome is a group of clinical disorders associated with a malignant disease and which are not a result of direct physical effects of the primary tumor or a metastatic disease [1]. It exists in 10-20% of patients, primarily in small cell lung, breast, ovarian cancer, and in malignant lymphomas; clinical manifestations differ. It is not related to the size of the primary tumor, it may occur late in the evolution of the disease or it may be the first sign of disease recurrence. The exact mechanism of occurrence of paraneoplastic syndrome is not clear, it is assumed to be related to the production of biologically active substances by tumors (polypeptide hormones and cytokines) or the production of antibodies. Paraneoplastic syndrome includes nonspecific metabolic and endocrine manifestations of a tumor. Symptoms and signs of paraneoplastic syndrome may be:
The literature gives the nephrotic syndrome as a direct cause of
thromboembolism due to loss of antithrombotic factors through urine
and increased production of prothrombotic factor in the liver [2]. CONCLUSION:The incidence of pulmonary thromboembolism has been
underestimated due to unreliable clinical picture, diagnosis, and
insufficiently accurate tests which would confirm clinically
suspected PTE. What is required here is a multidisciplinary approach
to the treatment because the real incidence is ten times higher than
estimated. The patient most likely had breast cancer with secondary
deposits but one which was detected late. PTE as a probable
consequence of paraneoplastic nephrotic syndrome was timely
diagnosed and treated. REFERENCE:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
|
Corresponding Address: Jasmina Mrgud, Internacionalni Dijaliza Centar Istočno Sarajevo E-mail: jasminaza@gmail.com |
Paper received: 8.10.2019. Paper Internet issues: 26.11.2020. |
|||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||