|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
| UDK 616.97-036.22-053.9 COBISS.SR-ID 16474121 |
Page 12 |
|||||||||||||||||||||||||||||||||||
|
Original paper Reasons of attendance by older patients to department of venereal diseases and their knowledge of sexually transmitted diseases Milan Bjekić (1) , Sandra Šipetić-Grujičić (2) , Hristina Vlajinac (2) (1) CITY INSTITUTE FOR SKIN AND VENEREAL DISEASES, BELGRADE; (2) INSTITUTE OF EPIDEMIOLOGY, FACULTY OF MEDICINE, UNIVERSITY OF BELGRADE ACKNOWLEDGMENT: This work was supported by the Ministry of Science and Technology of Serbia, through the Contract №175042 (2011-2014). |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | Abstract:
Introduction: Several studies have shown increasing rates of many
sexually transmitted diseases (STDs) in the population group aged 50
years and older, worldwide. Older persons usually know less about
STDs and HIV/AIDS than younger individuals. The aim of the present
study was to reveal why older patients seek venereologists’ help and
to assess their knowledge of STDs. Material and Methods: Data were
collected from consecutive patients aged 60 and over who attended
counselling for sexually transmitted diseases at the City Institute
for Skin and Venereal Diseases in Belgrade from July to December
2017. One dermatologist examined and interviewed all participants by
the use of a questionnaire. Results: Out of all participants (174
patients), 23.56% had some of STIs, 58.62% had some other genital
disorders and 17.82 came for counselling. The most frequent viral
STDs were acute and recurrent genital warts and recurrent genital
herpes, while the most frequent bacterial STD was syphilis. Out of
non STDs the most frequent were balanitis, in men, and lichen
sclerosis in both sexes. The perceived knowledge mean scores for
each STD, ranging from ”0”, meaning not knowledgeable at all, to
“5”, meaning very knowledgeable, ranged from 0.63 to 2.71. It was
the best for syphilis, followed by gonorrhoea, HIV/AIDS, hepatitis
B, genital warts and Chlamydia. Correct answers concerning general
knowledge of STDs were given by 59% to 96% of participants.
Conclusion: A considerable number of older people who sought
venereologists’ help had an STD. Their general knowledge of STDs as
well as perceived knowledge of single STDs were unsatisfactory and
did not differ between patients with and without STDs. Key Words: sexually transmitted diseases, genital disorders, HIV, counselling, elderly, knowledge of sexually transmitted diseases |
|||||||||||||||||||||||||||||||||||
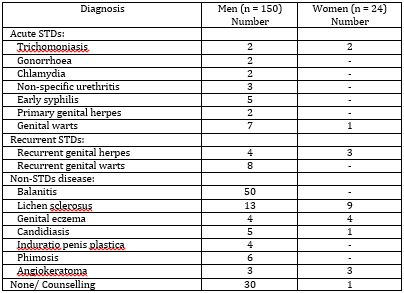
| INTRODUCTION: Sexually transmitted diseases (STDs) occur predominantly in individuals of younger age groups. Nonetheless, several studies have shown increasing rates of many STDs in the population group aged 50 years and older, worldwide [1-4]. Globally, the share of people aged ≥60 has risen from 8% (200 million people) of world population in 1950 to 11% (760 million) in 2011 and people older than 60 years are expected to reach 22% of world population (2 billion) by 2050 [5]. The situation in Serbia is similar: in the last six decades population aged 60-plus increased from 0.6 million in 1948 to 1.8 million in 2011 [6]. Sexual activity and the potential for STDs continue into late life. Several factors contribute to STD increase in older adults such as: increased longevity, better quality of life due to healthcare advancements, high divorce rates, being widowed, meeting new partners later in life, internet dating, effective pharmacotherapy for erectile dysfunction, no risk of pregnancy and lack of condom use during sex [4]. Moreover, older persons know less about STDs and HIV/AIDS than younger individuals because the elderly have been neglected by those responsible for education and prevention messages [7]. Genitourinary medicine departments predominantly target younger persons but are attended also by many older people. Epidemiological data about incidence of syphilis and gonorrhoea in Serbia in 2016 have shown that the lowest incidence rates were in patients older than fifty years (0.35 per 100,000 for syphilis and 0.11 per 100,000 for gonorrhoea) [8]. The objectives of our study were to reveal why older patients came to the Department for Sexually Transmitted Diseases at the City Institute for Skin and Venereal Diseases in Belgrade and to assess their knowledge of sexually transmitted diseases. METHODS: In this cross-sectional study, the data were collected from consecutive patients, both male and female, aged 60 and over who attended the Department for Sexually Transmitted Diseases at the City Institute for Skin and Venereal Diseases in Belgrade. This is the main institution for patients with sexually transmitted diseases in Belgrade, with a counselling department. The study was conducted between 1 July and 31 December 2017 and covered 174 patients. One dermatologist examined and interviewed all participants by the use of a questionnaire. Data on demographic characteristics (age, education, marital status), reasons for attendance, as well as sexual history data (sexual orientation, steady partner, human immunodeficiency virus (HIV) status, date of last sexual intercourse and condom use during this intercourse, number of sexual partners in past 6 months, and history of sexually transmitted diseases) were also collected. Diagnoses were made by physical and/or laboratory examinations. The participants’ knowledge of sexually transmitted diseases were assessed by a list of 14 questions (7 true and false questions and 7 Likert-style questions with responses ranging from not at all knowledgeable to very knowledgeable), taken from a study conducted by Andrea Jennings [9]. Data were presented as numbers and percentages. According to diagnoses, patients were divided into three groups: patients with STDs, with non-STDs and with no diagnoses. For the analysis of data, all participants were divided into two groups, group of patients with STDs and and group of patients without STDs. Throughout the analysis of differences between these groups, chi-square test and t- test were performed. P value <0.05 was considered as significant. The research was approved by the Ethics Committee of the City Institute for Skin and Venereal Diseases in Belgrade (the Ethics Committee approval number 3/2017). RESULTS: The study included 174 patients. Out of them 41 had an STd (26 acute STd and 15 recurrent STd), 102 patients had some other genital disorders and 31 persons visited the STD department for counselling (i.e. erectile dysfunction, drugs for erectile dysfunction, fear of STDs, lubricants) (Table 1). Among men, 23.3% had an STD, and among women 20.8%. The most frequent viral STDs were acute and recurrent genital warts and recurrent genital herpes, while the most frequent bacterial STD was syphilis. Out of non STDs the most frequent was balanitis, in men, and lichen sclerosus both in men and women.
Table 1. Reasons for attendance in the Department for Sexually
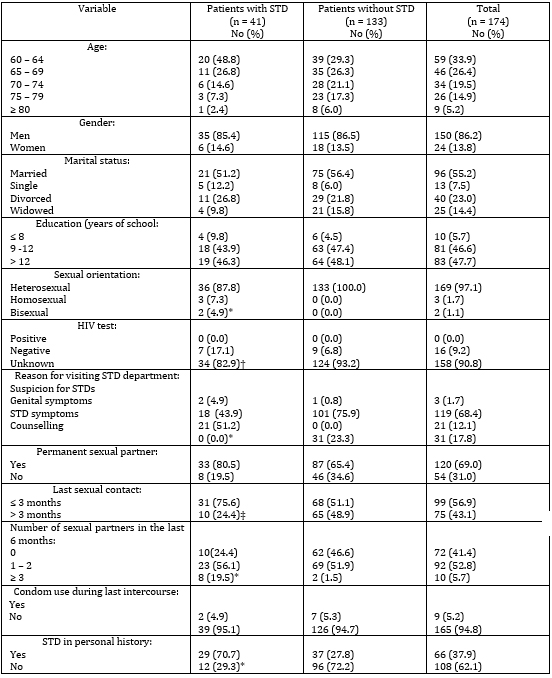
Transmitted Diseases For further analysis, all participants were divided into two groups: a) group of patients with STDs (41 patients) and b) group of patients without STDs which included both patients with some genital disorders and those coming for counselling (all together 133 persons). Their demographic and some other characteristics are presented in Table 2. Table 2. Some characteristics of the study
participants More than half of participants (63.3%) were 60-69 years old,
34.4% were 70-79 years of age and only 5.2% were 80 and more years
old. Majority of them were men (86.2%) with secondary (46.6%) or
university (47.7%) education and nearly half of them (44.9%) were
single, divorced or widowed. Only 5 (2.8%) patients declared as
homosexual or bisexual and 90.8% of all participants were never
tested for HIV. With the exception of 31 patients who visited STD
department for counselling, all others came because of genital
symptoms (68.4%), STD symptoms (12.1%) or suspicion of STIs (1.7%).
As much as 69.0% had a regular sexual partner and 56.9% had their
last sexual contact in the preceding 3 months. In the last 6 months,
41.4% had no sexual partner, 52.8% had 1-2 and only 5.7% had 3 or
more sexual partners. During the last intercourse, 94.8% of
participants did not use a condom. STD in personal history was
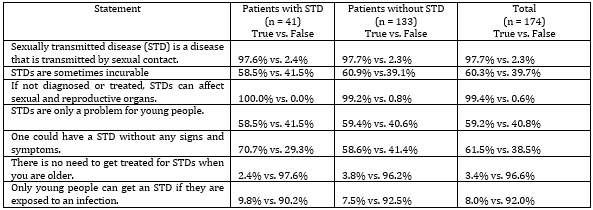
reported by 37.9% of participants. Table 3 General knowledge of sexually transmitted
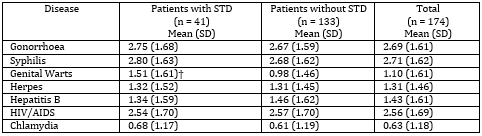
infections among study participant Perceived knowledge mean scores for single STD among the study participants (Table 4) ranged from 0.61 to 2.80. Perceived mean scores were the best for syphilis (2.71), gonorrhoea (2.69) and HIV/AIDS - acquired immunodeficiency syndrome (2.56), followed by hepatitis B (1.43), herpes (1.31) and genital warts (1.10), and the poorest for Chlamydia (0.63). There were no significant differences between patients with and without STDs. The only exception was perceived knowledge of genital warts which was better in patients with STDs in comparison with patients without STD (1.51 vs. 0.98, p<0.05). Table 4 Perceived knowledge mean scores* for
single sexually transmitted diseases among the study participants DISCUSSION: REFERENCES:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
|
Corresponding Address: Milan Bjekić, Gradski zavod za kožne i venerične bolesti, Dž. Vašingtona 17, Beograd E-mail: milinkovski@gmail.com |
Paper received: 15.1.2020 Paper Internet issues: 30.6.2020 |
|||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||