|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
| UDK 613-056.24:616-006 616.22-089.85 COBISS.SR-ID 16485129 |
Page 25 |
|||||||||||||||||||||||||||||||||||
|
Original paper Subjective assessment of the quality of life of laryngectomized patients before and after speech rehabilitation Mila Bunijevac (1,2), Neda Milošević (1, 3), Gordana Čolić (1), Dragan Čauševac (1,3), Ivana Ristić (4) (1)HIGH SCHOOL OF SOCIAL WORK, DEPARTMENT OF SPEECH THERAPY, BELGRADE, SERBIA; (2) PHI HOSPITAL "SVETI VRAČEVI", REPUBLIC OF SRPSKA, BIH; (3) CENTER FOR SPEECH PATHOLOGY - LOGOMEDIC, BELGRADE, SERBIA; (4) HIGH SCHOOL OF SOCIAL WORK, OCCUPATION THERAPY DEPARTMENT, BELGRADE, SERBIA |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | Abstract:
Introduction: Total laryngectomy exposes the patient to a great deal
of psychological stress, both because of the underlying disease and
the loss of a very important organ in the overall functioning of the
organism and organs, which enables an adequate communication
process. Objective: The aim of this study is to conduct a subjective
assessment of the quality of life of laryngectomized patients before
and after vocal rehabilitation. Methods: The study involved 50
patients after total laryngectomy, ranging in age from 51 years to
83 years. A subjective assessment of speech and voice was conducted
with the University of Michigan Quality of Life Instrument — HNQOL
and Voice Handicap Index — VHI. These instruments provide
information from the patient about the treatment or treatment
applied, as well as the impact that vocal rehabilitation has on the
quality of his or her life before and after treatment. Results:
Prior to vocal rehabilitation of the HNQOL scale, patients
experienced pronounced difficulties on all subscales, especially
when it came to communication ( E(x)= 5.75 ± 8.64) and emotions (
E(x)= 16.66 ± 15.17); expressed, while chewing/food ingestion ( E(x)=
53.91 ± 26.45) and pain ( E(x)= 50.50 ± 17.71) had mean values. VHI
scale (physical subscale E(x)= 36.6 ± 2.93; emotional subscale E(x)=
34.96 ± 3.79; functional subscale E(x)= 35.64 ± 3.37) before vocal
rehabilitation, all subjects (100%) belonged to the third category
(severe handicap), which was a problem when it came to psychosocial
functioning. After vocal rehabilitation, the mean values on the
HNQOL scale were very highly expressed and statistically highly
significantly improved (communication E(x)= 93.37 ± 10.28; emotions
E(x)= 90.58 ± 8.23; chewing/swallowing food E(x)= 96.66 ± 5.77; pain
E(x)= 92.25 ± 6.98) which indicated a good quality of life. On the
VHI scale of low value (physical subscale E(x)= 10.84 ± 4.41;
emotional subscale E(x)= 4.42 ± 4.63; functional subscale E(x)=
21.32 ± 13.29) shows a statistically high significant improvement,
ie good psychophysical and functional condition patient. Conclusion:
Subjective assessment after vocal rehabilitation resulted in
improvement of all parameters tested, especially in the domain of
communications and emotions.Vocal rehabilitation has had a positive
effect on improving the quality of life of these patients,
integrating them into the family and the environment, as well as
performing daily activities that we observe through their physical,
emotional and functional state. Keywords: Larynx tumor, Total laryngectomy, Quality of life, HNQOL scale, VHI scale. |
|||||||||||||||||||||||||||||||||||
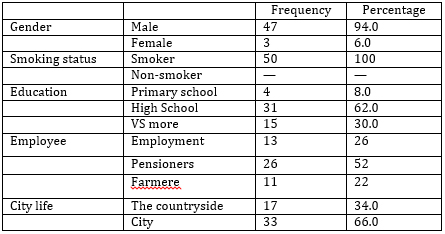
| INTRODUCTION Total laryngectomy is a radical procedure that results in the permanent loss of the generator and part of the resonator of the voice, the larynx in which the underlying laryngeal tone is created [1]. Total laryngectomy is performed in advanced cases of laryngeal cancer with signs of deep laryngeal infiltration (T3) or in tumors that have spread to adjacent organs (T4), ie when all the potential for partial surgery is exhausted (2, 3). The patient is exposed to a great deal of psychological stress, both because of the underlying illness and the loss of a very important organ in the overall functioning of the organism and the organ participating in the exercise of communication [4]. Total laryngectomy leads to physical and functional changes that can affect the emotional state and some of the most basic life functions, including breathing, swallowing and communication [5]. Speech rehabilitation is a complex and active process that requires the involvement and cooperation of a laryngectomized person and speech therapist. Speech is an expression of social activity because it is realized in communication with other people. Rehabilitation of laryngeomized patients modifies the anatomy of the upper aerodigestive pathways, creating new anatomical conditions on which breathing, swallowing and phonation functions will have to be organized [3]. It is a very important form of rehabilitation, which in addition to successfully mastering one of the methods of speech increases confidence, creates a better sense of security and improves quality of life [6], The basic possibilities of speech rehabilitation after total laryngectomy are the development of esophageal speech skills, treoesophageal puncture with the use of a vocal prosthesis, and the use of electrolarynx. Quality of life has been conceptualized as a multidimensional concept in which health, well-being, health comprehension, functional status and life choices overlap [7, 8]. Some define quality of life in cancer patients as the difference between patient expectations and low achievement that affect quality of life improvement [9]. Quality of life is a general well-being that encompasses objective factors and a subjective evaluation of physical, material, emotional and social well-being, including personal development and purposeful activities [10]. Basic aspects of quality of life are health, functional ability, life satisfaction and independence [11]. It can be measured using a variety of questionnaires, which are mostly completed by patients and thus gives an opinion on the experience of their speech and voice when it comes to physical, emotional and functional state. The quality of life of patients after total laryngectomy is studied within the oncology of head and neck tumors, because of all malignant tumors of the head and neck, laryngeal cancer is the most common cause of oral cancer and oropharynx. The aim of this study is to examine the quality of life of laryngectomized patients before and after vocal rehabilitation. METHODS The study involved 50 patients after total laryngectomy, ranging in age from 51 years to 83 years. The research was conducted at SWU "SvetiVračevi" Hospital in Bijeljina and the Military Medical Academy in Belgrade from April 2014 to November 2015. Data on gender, age, education, smoking experience, time when rehabilitation was initiated, vocal rehabilitation model, and length of treatment were collected through a questionnaire and interview with a patient. A subjective voice assessment was conducted with University of Michigan Quality of Life Instrument instruments - HNQOL, Terrell et al. [12] and the Voice Handicap Index - VHI, Jacobson et al. [13]. University of Michigan Quality of Life Instrument -HNQOL scale is used to evaluate the quality of life of patients with head and neck cancer. It has been translated into many languages and adapted to different cultures. It was adapted for our speech area by Petrovic-Lazic, Bunijevac in 2014. The scale contains 30 questions, 20 of which are used to score four domains of quality of life assessment: communication (4 points), chewing/swallowing food (6 points), pain (4 points) and emotions (6 points). Respondents were tasked with selecting the answer given for each of these questions, expressing their feelings and opinions about the possibility or success of communication, the possibility of chewing / swallowing food, pain and emotional state. The HNQOL scale can also be used to assess a patient's satisfaction with treatment or treatment, as well as the impact of speech rehabilitation on the quality of his or her life before and after treatment. Voice Handicap Index - The VHI scale is used to measure the therapeutic outcome of vocal rehabilitation as well as to evaluate the severity of a voice problem. The VHI scale covers three areas, namely: P — physical, E — emotional, F — functional. Each area contains 10 questions. Respondents were tasked with selecting the answer given for each question: "never", "almost never", "sometimes", "almost always", "always". In this way, they expressed their opinions about the experience of their voice and speech when it comes to physical, emotional and functional state. The VHI scale can provide information about the degree of speech disability experienced by the patient himself and the impact that vocal rehabilitation has on the quality of his or her life before and after treatment. Data were collected on two occasions. Patients completed the questionnaire the first time they came to the speech therapist, before starting treatment and the second time after completing the treatment. Descriptive measures, arithmetic mean with associated standard deviation, as well as minimum and maximum were used in the statistical data processing. Frequency and percentages, and t-test for dependent samples were used. Statistical analysis and analysis were done in the SPSS version 20 (Statistical Package for the Social Sciences) computer program. RESULTS The study involved 50 patients after total laryngectomy, 47 male subjects and three female subjects, as shown in Table 1. All subjects in this study were smokers. The most frequently represented respondents were pensioners, slightly fewer were persons in employment, and these were mostly persons with secondary education. The examiners came from both urban and rural areas.
Table 1.Structure of the sample by gender, smoking status, education
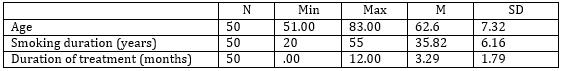
and place of residence The age of the respondents ranged from 51 to 83 years (Table 2). The length of smoking experience ranges from 20 to 55 years, and the length of treatment ranges from one month to 12 months. Table 2.Structure of the sample by age of the
respondent, length of smokers' time and length of treatment Patients mastered two models of speech, namely esophageal and electro-laryngeal speech (Table 3). Table 3. Structure of the sample according to
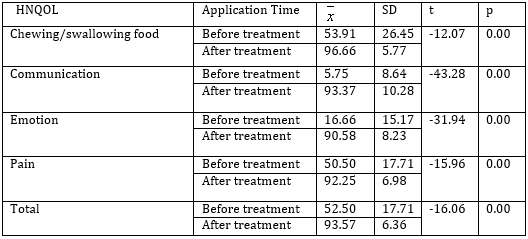
vocal rehabilitation model Prior to vocal rehabilitation, the HNQOL subscales had low levels of expression on the HNQOL subscale, especially with regard to communication and emotion subscales, whereas the subscales related to food ingestion and chewing and pain had medium levels. Using the t-test for dependent samples after vocal rehabilitation, statistically significant improvement was found on all subscales of the HNQOL scale (Table 4). A statistically significant difference on the HNQOL scale also exists in the total score before and after treatment, which means that better overall functioning of patients in all examined domains after treatment compared to the pre-treatment period, which also indicated a better quality of life. Table 4.HNQOL scale — before and after vocal
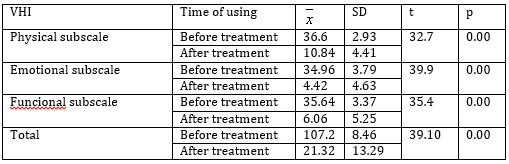
rehabilitation Prior to vocal rehabilitation on all subscales of the VHI scale,
subjects had high mean values, which negatively affected their
quality of life. Using the t-test for dependent samples after vocal
rehabilitation, statistically significant improvement was found on
all subscales of the VHI scale, that is, the patients' physical,
emotional and functional condition improved after treatment (Table
5). Table 5.VHI scale — before and after vocal
rehabilitation DISCUSSION REFERENCES:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
|
Corresponding Address: Mila Bunijevac, Visoka škola Socijalnog rada, Departman za Logopediju, Beograd E-mail: bunijevacmila@yahoo.com |
Paper received: 3.4.2020 Paper Internet issues: 30.6.2020 |
|||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||