|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
| UDK 616-008.9:577.152.3 COBISS.SR-ID 16549897 |
Page 68 |
|||||||||||||||||||||||||||||||||||
|
Case report Macroamylasemia as a cause of hyperamylasemia in clinically unclear conditions-case report Zoran Joksimović (1) , Dušan Bastać (2) , Snežana Pavlović (3) (1) INTERNIST PRACTICE "JOKSIMOVIĆ" BOR, (2) INTERNIST'S OFFICE "DR. BASTAĆ" ZAJEČAR; (3) SPECIALIST PRACTICE FOR INTERNAL MEDICINE "DR PAVLOVIĆ CARDIOLOGY" BELGRADE |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | Abstract:
Macroamylasemia is a rare condition characterized by elevated serum
amylase levels due to the existence of macromolecules - complex
amylase that cannot be secreted normally by the kidneys due to their
size. It is a benign condition that is usually free of marked
clinical symptoms and signs. The prevalence of macroamylasemia in
the population is between 1 and 2%. The main clinical significance
of macromylasemia is that it is often a diagnostic problem because
it requires differentiation of this condition from other causes of
hyperamylasemia. Therefore, it is rational to avoid unnecessary
diagnostics and treatment, which burden both the patient and the
health system. Macromalasemia as a diagnosis should be considered in
any patient with elevated serum amylase activity in whom serum
lipase and urine amylase levels are normal. Laboratory confirmation
of the diagnosis of amylasemia rests on tests: electrophoresis or
polyethylene glycol precipitation test. This paper presents a
patient who has been routinely treated clinically due to
non-specific gastrointestinal problems. During laboratory treatment,
the patient's serum was found to have elevated amylase values.
Additional diagnostics did not identify organic pancreatic diseases
or other diseases that may be related to hyperamylasemia, and by
calculating the ratio of renal amylase clearance to creatinine
clearance of less than 1%, we conclude that it is most likely a
macroamylasemia. Specific treatment was not required. The patient
comes for a check-up once every 6 months. |
|||||||||||||||||||||||||||||||||||
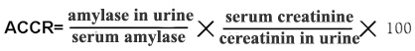
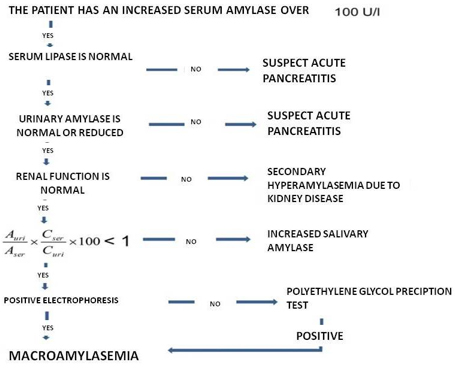
| INTRODUCTION: Amylase is an amylolytic enzyme that helps digestion in the intestines by hydrolyzing polysaccharides to smaller molecules. In humans, there is α-amylase, which in healthy individuals originates mostly from the pancreas and salivary glands, but in clinically insignificant amounts from other organs (liver, kidneys, fallopian tubes, muscles, etc.). It can be found in two basic forms, the so-called isoenzymes - synthesized in the pancreas (pancreatic or P-isoamylase) and non-pancreatic origin (salivary - salivary or S-isoamylase). It is common to have low levels of amylase in the blood or urine. But if the pancreas or salivary glands are damaged, the level of amylase in the blood or urine increases. Serum amylase is elevated in at least 75% of cases of pancreatitis; Rarely, serum amylase may be normal, even if massive pancreatic necrosis occurs [1] The detailed pathways of serum amylase metabolism have not yet been fully elucidated. Decreased metabolic clearance - renal failure may be the cause of elevated serum amylase levels. People who have had a nephrectomy or have kidney failure have an average serum amylase level that is 50% higher than healthy individuals. Therefore, it can be assumed that the kidneys play a major role in amylase metabolism. However, the kidney is not the only organ responsible for removing amylase in humans. The extrinsic mechanisms of amylase clearance are not clearly defined. Since high serum amylase levels are also observed in liver necrosis and cirrhosis, the liver is thought to play a role in amylase metabolism [2] Many conditions have been reported to cause hyperemylasemia. Although hyperamylasemia is usually assumed to be a consequence of the release of serum amylase by the diseased organ, the precise relationship between hyperemylasemia and pathological conditions is not entirely clear. Hyperamylasemia is most often the result of: pancreatitis or mumps, decreased metabolic clearance of amylase or amylase released from a damaged organ (outside the pancreas and salivary glands). Acute or chronic pancreatitis is associated with an increase in type P isoamylase. Other causes of hyperemylasemia associated with pancreatitis are pseudocysts, pancreatic trauma, and choledolithiasis. Pancreatic trauma can be the result of blunt trauma, abdominal or retroperitoneal surgery, or endoscopic retrograde pancreatic canal cannulation (ERCP). In patients with biliary colic-type abdominal pain, a threefold increase in serum amylase levels returns to normal within 48-72 hours. suggests the passage of a stone through the common bile duct [3,4]. Mumps due to infection, trauma or radiation is associated with an increase in type S isoamylase. Salivary gland damage can also occur as a consequence of chronic alcoholism. The level of amylase in saliva is three times higher than normal in 10% of patients treated for chronic alcoholism. It is also discussed that this phenomenon in alcoholics is a consequence of and / or liver damage because liver disease (hepatitis or cirrhosis) also shows elevated levels of isoamylases of type S and P [2]. Intestinal diseases (inflammatory bowel diseases, infarct mesentery, ileus, peritonitis) can lead to increased levels of pancreatic amylase. Ruptured ectopic pregnancy, ovarian cysts, or inflammation of the ovaries and fallopian tubes can result in elevated salivary isoamylase. Ectopic amylase production is possible in malignancies of the lungs, ovaries, pancreas, and colon; pheochromocytoma; team; multiple myeloma, breast cancer. Increases in amylase levels may occur postoperatively, after extracorporeal circulation or non-abdominal surgery (e.g., 30% of patients undergoing cardiac surgery have elevated type C isoamylase). Rare cases of hyperamylasemia have been reported with ciprofloxacin treatment. Other causes of hyperamylasemia include pneumonia, cerebral trauma, burns, abdominal aortic aneurysms, anorexia nervosa, and organophosphate poisoning. (5,6) Elevated pancreatic enzymes can be found in critically injured patients with trauma even if there is no true pancreatitis [1,2]. Macroamylasemia - Macroamylasemia is a rare, benign condition in which the amylase molecule binds to large complex molecules, reducing renal clearance and prolonging its half-life. The prevalence of macroamylasemia in the population is between 1 and 2%. About 2% -5% of patients with hyperamylasemia have macroamylalasemia. Macroamylasamia is characterized by hyperamylasemia or elevated serum amylase levels without elevated urine amylase and other clinical signs or symptoms. In macroamylasmia, amylase is most often bound by immunoglobulin, making it 4 times larger than usual and the kidneys excrete it slowly and with difficulty, resulting in high serum amylase levels but normal urine levels [7-12]. In most cases, macromolecular amylase is a complex of normal amylase and immunoglobulin A or G. Different papers report different statistics on the incidence of macroamylasemia. It is most often present in adults (more often males), although cases have been reported in children and newborns. Elevated serum amylase levels are the main criterion for the diagnosis of pancreatitis. health system. This is important, among other things, because the main limitation of the use of serum amylase measurements in the diagnosis of the degree of pancreatitis is the lack of specificity of this test [1,7,13]. An accepted algorithm for the joint diagnosis of macroamylasemia, in elevated serum amylase without elevated urinary amylase, is subsequent serum lipase testing, which together with high amylase levels usually suggests pancreatitis [14]. If serum lipase is normal, renal function must be examined. because abnormal kidney function will also cause elevated amylase levels. Then when we conclude that renal function is normal, we should calculate the renal amylase clearance in relation to creatinine clearance - ACCR (Amylase-creatinine clearance ratio) according to the formula:
The normal ratio of these clearance is between 3% and 5%, while a
result of less than 1% suggests macroamylasemia [13]. The final
confirmatory test is electrophoresis or polyethylene glycol
precipitation test and chromatography [14]. As these are methods
used in specialized laboratories and are rarely used routinely, most
authors agree that the calculation of ACCR ratios can be considered
diagnostic, although there are some discrepancies that [7,13,15,16].
Conclusion: In our patient, based on the clinical picture,
performed diagnostics and calculated ACCR, we conclude that it is
most likely macroamylasemia. These simple and inexpensive laboratory
tests and calculations confirmed the diagnosis despite the lack of a
confirmatory laboratory test (Definitive diagnosis by
electrophoresis or polyethylene glycol precipitation test was not
available to us and the patient was not motivated for additional
diagnosis). With the recommended diet and therapy, the patient was
without any problems. Due to age, a colonoscopy was suggested, which
the patient refused. A control clinical examination and ultrasound
examination of the abdomen are scheduled for 6 months. REFERENCES:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
|
Corresponding Address: Joksimović Zoran, INTERNISTIČKA ORDINACIJA „JOKSIMOVIĆ“ BOR, Srbija E-mail: joksaza@ptt.rs |
Paper received: 18.3.2020 Paper Internet issues: 30.6.2020 |
|||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||