| |
|
|
INTRODUCTION
Metabolic syndrome (MetS) is a cluster of several disorders and
includes abdominal obesity, dyslipidemia of HDL and LDL cholesterol,
elevated triglycerides, elevated blood pressure, glucose intolerance
or type 2 diabetes [1]. The term cardiometabolic syndrome has been
used increasingly. According to the NCEP-ATPIII -2001 classification
and harmonized definition [1] metabolic syndrome exists if three of
the five risk factors are positive:
- 1. Abdominal obesity-waist circumference in men ≥ 94 cm
(previously >102 cm), and in women ≥80 cm ( previously >88 cm)
- triglycerides higher than 1.9 mmol / L ( > 1.7 mmol/L )
- HDL cholesterol lower than 1.1 mmol / L (1 , 2 ; 1,4)
- glycemia higher than 5.6 mmol / L
- blood pressure >130/85 mmHg or higher
MetS is characterized by the simultaneous presence of obesity,
hypertension, dyslipidemia, and hyperglycemia in an individual,
which leads to an increased risk of cardiovascular disease (CVD). It
affects nearly 35% of the US adult population, and its prevalence
increases with age. Elevated blood pressure is an almost regular
component of the metabolic syndrome; however, optimal
antihypertensive therapy has not yet been defined [2].
Abdominal obesity, glucose intolerance, hypertension and diabetes
synergistically interact and lead to left ventricular remodeling.
These facts may explain the significantly increased risk of heart
failure with preserved ejection fraction and cardiovascular disease
when these factors are grouped together [3].
Left ventricular hypertrophy (LVH) is thickening of the wall of the
heart muscle - hypertrophy of cardiomyocytes and hyperplasia of
connective tissue, the consequence of which is a decrease in the
volume of the ventricles in concentric hypertrophy, which is typical
for hypertension with the participation of non-hemodynamic factors
(genetics, stress, other external factors) as well. [4]. The
consequences of concentric hypertrophy are: left ventricular
diastolic dysfunction with preserved left ventricular ejection
fraction, reduction of longitudinal systolic function, electrical
instability (arrhythmias) and subendocardial microvascular ischemia
(Figure 1).
Figure 1. taken from https://remixeducation.in/case-of-ischemic-heart-disease-hid/

Eccentric and dilatational hypertrophy (elongation of
cardiomyocytes via sarcomere replication) increases chamber volume
and is typical for athletes but also occurs in obesity and volume
overload. A more severe degree of myocardial hypertrophy (Figure 2)
increases overall cardiovascular risk and mortality (congestive
heart failure, sudden cardiac death). LVH is an independent
prognostic factor and lethal marker of hypertension.
Figure.2. Echocardiographic image of a patient
with extreme LVH of 345 g

Metabolic syndrome, which essentially includes insulin
resistance, hyperinsulinemia, and hyperglycemia, alters myocardial
metabolism and promotes myocardial inflammation, fibrosis, and left
ventricular remodeling [5-8]. The ejection fraction of the left
ventricle is most often preserved in metabolic syndrome and diabetes
because the altered metabolic milieu leads to remodeling of the
heart cavities, left ventricular hypertrophy and diastolic
dysfunction, but also to subtle impairment of systolic function,
which is detected through longitudinal global strain
echocardiography [5-9]. For these reasons, the development of left
ventricular hypertrophy doubles the risk for heart failure with
preserved ejection fraction.
OBJECTIVE:
Determination of the impact of obesity to the incidence and
degree of severity of myocardial hypertrophy in hypertensive
patients with metabolic syndrome in comparison with the control
group - hypertensive patients without metabolic syndrome.
PATIENTS AND METHODS
Consecutive patients of the Office of internal medicine "Dr.
Bastać" were examined, a total of 55 patients with hypertension, who
were divided into two groups:
- with metabolic syndrome N=22 (40%) patients , 10 male and 12
female, average age 56 ± 8.5 years with BMI>30kg/m 2 and waist
circumference higher than 80 cm for females and > 94cm for men
- control group without metabolic syndrome 33 (60%) 11 male
and 22 female, average age 52 ± 14 years, with BMI<30 kg / m 2
Body mass index (BMI in kg/m2 ) in the control group is 24.9±3
kg/m2 , and in the examined group 32.5±2.5 kg/m2 , a highly
statistically significant difference is evident in body weight
(p<0.001)
The number of cardiovascular risk factors that make up metabolic
syndrome in the individual distribution was in the study group with
metabolic syndrome - study group (N = 22 pts)
- 5 factors - 5 patients (22%)
- 4 factors - 8 patients (36%)
- 3 factors - 9 patients (42%)
It was not possible to observe other factors, e.g. parameters of
systemic inflammation (hsCRP, interleukins, etc.) and measurement of
insulin resistance (HOMA index, insulinemia during the OGTT test,
etc.).
All patients had standard biochemical results, including serum
concentrations of lipid fractions and blood glucose.
Echocardiography was done for all subjects on a Power Vision 6000
Toshiba echo camera with standard echocardiographic measurements in
the M, B and Doppler technique, and the mass of the left ventricular
myocardium was determined for them using the Devereux formula [10]:
LVM(g)= ((EDD+IVSd+PWd)**3 - EDD**3 ) x 1.05
-13.4
Also, myocardial mass is indexed to the body surface and
myocardial mass index-LVMI (g/m2 ) is obtained.
The echocardiographic criterion for normal myocardial mass is up to
224g for men and 162g for women, on average less than 193g for both
sexes. Normal myocardial mass index is less than 95 g/m² for women,
less than 115 g/m² for men, on average less than 105 g/m².
Statistical processing was done through descriptive processing, for
attributive characteristics using chi-squared test, and for
numerical ones the Student's T test, both by means of the Mikrostat
program.
RESULTS
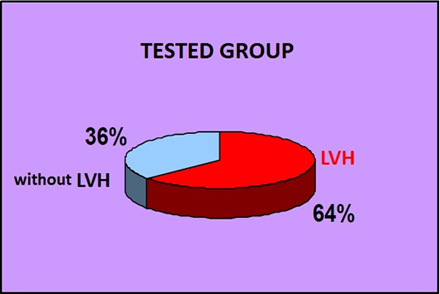
Individual distribution - prevalence of left ventricular
hypertrophy (LVH) in groups (for women LVMI >95 g/m2 and for men
LVMI >115 g/m2) is shown in Chart 1.
CHART 1a. Prevalence of LVH in the group with
metabolic syndrome and hypertension
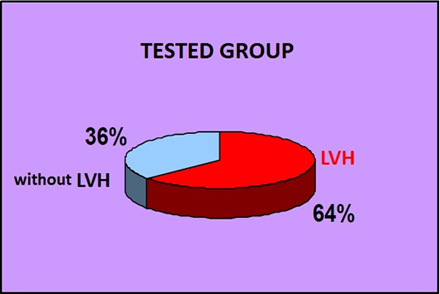
CHART 1b. Prevalence of LVH in the group with
hypertension without metabolic syndrome

In the examined group 64% had LVH (Chart 1a), while in the
control group 36 % had it (Chart 1b).
There is a statistically significantly higher number of patients
with LVH in hypertension with metabolic syndrome compared to
hypertensive patients of the control group without metabolic
syndrome (X2 , p = 0.027)
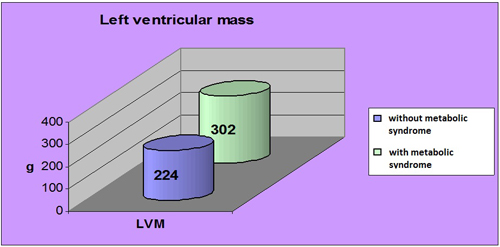
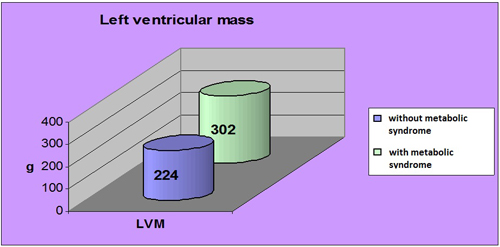
In the group of hypertensive patients with metabolic syndrome, the
degree of severity of myocardial hypertrophy ie. myocardial mass is
statistically significantly higher compared to the control group
(respectively 302±84g versus 224±89g , p=0.0002) (Graph 2.)
Graph. 2. The degree of severity of hypertrophy -
left ventricular myocardial mass in grams (g) in relation to the
presence of metabolic syndrome
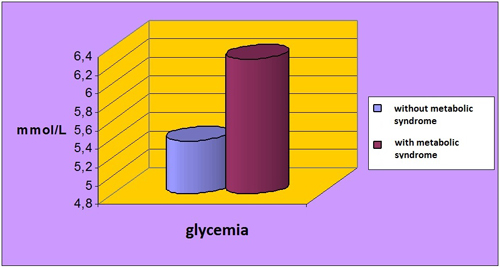
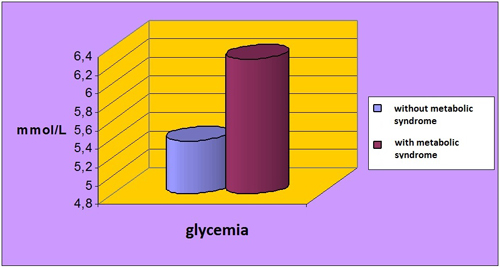
Glycemia values are slightly elevated in hypertensive patients
with metabolic syndrome, on average 6.1 mmol/L, and in hypertensive
patients without metabolic syndrome, they are normal at 5.5 mmol /
L. (p<0.05) (Graph 3.)
Graph. 3. Glycemia values in hypertensive patients
with and without metabolic syndrome
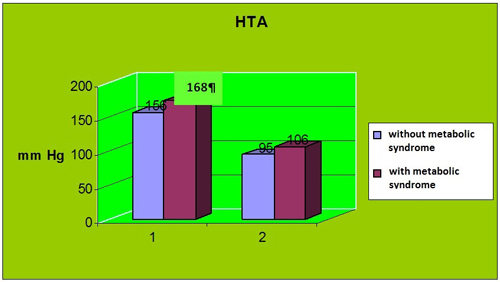
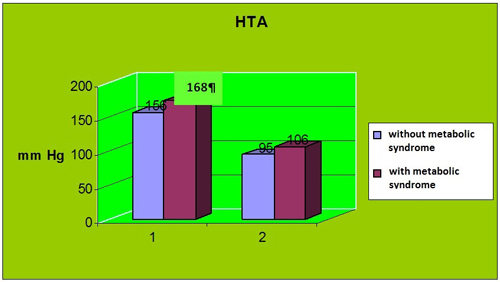
Arterial pressure values were higher for both systolic and
diastolic blood pressure 168/106 mmHg in hypertensive patients with
metabolic syndrome, but did not reach statistical significance in
relation to blood pressure values in hypertensive patients without
metabolic syndrome (156/95 mmHg, p=0.16 ) (Chart 4).
Graph 4. Arterial pressure values in hypertensive
patients with and without metabolic syndrome
DISCUSSION
The prevalence of left ventricular hypertrophy (LVH) in the
examined group with metabolic syndrome (MetS) was quite high (64%),
almost twice as high as the prevalence of the control group with
isolated hypertension (36%). In the Second Strong heart study, De
Simone et al. out of 1648 patients, they found 406 (25%) patients
with LVH [11], which is a much lower number. We explain this
difference by the fact that it is difficult to compare the given
data, due to different patient selection factors, as well as genetic
predisposition for hypertrophy. It is evident that the prevalence of
hypertrophy is higher in our group because there were more severe
patients with more metabolic syndrome factors. In patients without
MetS with hypertension, our result of the prevalence of myocardial
hypertrophy is 36%, while in the 2nd Strong Heart there were only
13% of subjects with LVH, which can be explained by the fact that
they were without hypertension and that it was physiological
hypertrophy or incipient hypertrophic cardiomyopathy [12]
Von Jensen et al. [3] in a population cohort study of 5741
participants of the Framingham study published in 2020, state that
the prevalence of LVH is increased in subjects with associated
hypertension, obesity and diabetes. Also, MetS and diabetes affect
the reduction of left ventricular ejection fraction (LVEF), which is
not the case when there is hypertension with MetS without diabetes.
In our group of hypertensive patients with MetS, the degree of
severity of myocardial hypertrophy, i.e. myocardial mass is
statistically significantly higher compared to the control group
(respectively 302±84g versus 224±89g, p=0.0002). On average, the
contribution of the metabolic syndrome gives a higher myocardial
mass by 26% than in hypertension without the metabolic syndrome,
while this increase in the Von Jensen study of 36% is comparable
because it was done on a very large sample [3]. In both, differences
are highly statistically significant for the impact of metabolic
syndrome on the increase in myocardial mass.
Arterial pressure values were higher for both systolic and diastolic
blood pressure 168/106 mmHg in hypertensive patients with MetS, but
did not reach statistical significance in relation to blood pressure
values in hypertensive patients without MetS (156/95 mmHg, p=0.16).
Given that the mean values of arterial pressure do not differ
between groups, it is concluded that non-hemodynamic factors for the
development of myocardial hypertrophy: abdominal obesity,
hyperglycemia, insulin resistance and dyslipidemia associated with
hypertension synergistically affect cardiac remodeling in terms of a
more severe degree of left myocardial hypertrophy chambers. Similar
conclusions are drawn on a large sample by von Jensen et al. [3].
These findings may explain the significantly increased risk of heart
failure and cardiovascular disease when these factors are grouped
together and play an important role in the induction of a more
severe degree of myocardial hypertrophy in hypertensive patients
with metabolic syndrome.
Metabolic syndrome (MetS) is associated with an increased prevalence
of electrocardiographically and echocardiographically determined (LVH)
and is a powerful predictor of cardiovascular outcome [11]. LVH is a
strong predictor of composite fatal and nonfatal cardiovascular
events over 8 years of follow-up, either in the presence or in the
absence of the metabolic syndrome, and accounts for a significant
portion of the high CV risk associated with MetS [11].
In the study by von Jeinsen B. et al. [3], 5741 participants of the
Framingham study were examined who underwent echocardiographic
measurements of left ventricular mass (LVM), ejection fraction (LVEF)
and global longitudinal strain (GLS) through multivariable
regression analysis. Statistically significant differences were
obtained between BMI category, hypertension and diabetes with LVH,
LVEF and GLS (p <0.01). Obesity, hypertension and diabetes status
were individually and jointly associated with greater severity of
left ventricular hypertrophy (LVM) and worse GLS (p<0.01 for all).
Obesity, hypertension and diabetes synergistically affect cardiac
remodeling. These findings may explain the significantly increased
risk of heart failure and cardiovascular disease when these factors
are grouped together in the metabolic syndrome [3].
Determining the etiology of left ventricular hypertrophy (LVH) can
be a challenge due to the similarity of various manifestations in
clinical presentation and morphological characteristics [12,13].
Patients with LVH remain asymptomatic for several years, but disease
progression will lead to the development of systolic or diastolic
dysfunction and end-stage heart failure. Distinguishing individuals
with treatable causes of LVH is important for the prevention of
cardiovascular events and mortality. An athlete's heart with
physiological LVH does not require treatment [13] The most common
causes of hypertrophy, usually concentric type, include etiologies
due to pressure overload, such as systemic hypertension, less common
aortic valve stenosis and very rarely infiltrative heart diseases
such as amyloidosis, Fabry disease and sarcoidosis. Volume overload
is common in aortic and mitral insufficiency and extreme obesity
[12,13].
Concentric myocardial hypertrophy occurs as a compensatory mechanism
for pressure overload in hypertension [14-16]. Myocyte hypertrophy
is associated with interstitial fibrosis, changes in cardiomyocyte
metabolism, myocyte apoptosis, and microvascular dysfunction. These
myocardial changes in hypertension are manifested as pathological
remodeling of the left atrium and left ventricle accompanied by
diastolic dysfunction, LVH and subtle myocardial systolic
dysfunction, while LVEF is initially preserved [14-17]. Thus,
obesity, diabetes mellitus and arterial hypertension cause LVH, but
it is still not entirely clear how their joint presence can affect
cardiac structure, function and ventricular geometry [17-35].
Finally, the results of epidemiological studies in the last 30 years
have shown that visceral adipose tissue, precisely measured by CT or
MRI, is an independent marker of the risk of cardiovascular and
metabolic morbidity and mortality [36]. Emerging evidence also
suggests that ectopic fat deposition, including hepatic and
epicardial fat, may contribute to increased atherosclerosis and
cardiometabolic risk.
CONCLUSION
Patients with metabolic syndrome and hypertension have a
statistically significantly higher prevalence of myocardial
hypertrophy compared to the control group of hypertensive
individuals without metabolic syndrome. The degree of myocardial
hypertrophy of the left ventricle is statistically significantly
higher compared to hypertensive patients without metabolic syndrome
.
Given that mean values of arterial pressure do not differ between
groups, it is concluded that non-hemodynamic factors for the
development of myocardial hypertrophy play an important role in the
induction of a more severe degree of myocardial hypertrophy in
hypertensive patients with metabolic syndrome. Abdominal obesity,
hyperglycemia and insulin resistance associated with hypertension
synergistically affect heart remodeling in terms of a more severe
degree of left ventricular hypertrophy than in hypertension without
metabolic syndrome. These results may partly explain the
significantly increased risk of heart failure and cardiovascular
disease when the metabolic syndrome, including obesity, prediabetes
or diabetes, dyslipidemia and hypertension factors are grouped
together.
LITERATURE:
- Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI,at
al. Harmonizing the metabolic syndrome: a joint interim
statement of the International Diabetes Federation Task Force on
Epidemiology and Prevention; National Heart, Lung, and Blood
Institute; American Heart Association; World Heart Federation;
International Atherosclerosis Society; and International
Association for the Study of Obesity. Circulation.
2009;120(16):1640-5. doi: 10.1161/CIRCULATIONAHA.109.192644.
Epub 2009 Oct 5. PMID: 19805654.
- Katsimardou A., Imprialos K., Stavropoulos K., Sachinidis
A., Doumas M., Athyros V. Hypertension in Metabolic Syndrome:
Novel Insights. Curr Hypertens Rev. 2020;16(1):12-18. doi:
10.2174/1573402115666190415161813.
- Jeinsen BV, Vasan RS, McManus DD, Mitchell GF, Cheng S,
Xanthakis V. Joint influences of obesity, diabetes, and
hypertension on indices of ventricular remodeling: Findings from
the community-based Framingham Heart Study. PLoS One.
2020;15(12):e0243199. doi: 10.1371/journal.pone.0243199. PMID:
33301464; PMCID: PMC7728232.
- Bastac D. et al. Differences in Left-Ventricular geometric
Remodeling induced by Hypertension and Obesity .. Int J Obes
2001;25 (Suppl 3): S31–S32.
https://doi.org/10.1038/sj.ijo.0801878 .
- Lorenzo-Almoros A, Tuñón J, Orejas M, Cortés M, Egido J,
Lorenzo Ó. Diagnostic approaches for diabetic cardiomyopathy.
Cardiovasc Diabetol. 2017;16(28):1–11. 10.1186/s12933-017-0506-x
- Varma U, Koutsifeli P, Benson VL, Mellor KM, Delbridge LMD.
Molecular mechanisms of cardiac pathology in
diabetes—Experimental insights. BBA—Mol Basis Dis.
2018;1864(5PtB):1949-1959. doi: 10.1016/j.bbadis.2017.10.035.
- Marwick TH, Ritchie R, Shaw JE, Kaye D. Implications of
Underlying Mechanisms for the Recognition and Managment of
Diabetic Cardiomyopathy. J Am Coll Cardiol. 2018;71(3):339–51.
10.1016/j.jacc.2017.11.019
- Hölscher ME, Bode C, Bugger H. Diabetic Cardiomyopathy: Does
the Type of Diabetes Matter? Int J Mol Sci. 2016;16:1–11.
10.3390/ijms17122136
- Bastać D., Raščanin A., Bastać M. Da li će globalni
longitudinalni strejn kao superiorni parametar sistolne funkcije
potpuno zameniti ejekcionu frakciju leve komore u proceni
hipertenzivne hipertrofije? Srce i krvni sudovi (Heart and Blood
Vessels Journal of the Cardiology Society of Serbia)
2019;38(3):124. Dostupno na:
http://uksrb.rs/uploads/sazetci%20XXII%20INT%20sks%2003%202019%2038%203.pdf
- Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E,
Sachs I, et al. Echocardiographic assessment of left ventricular
hypertrophy: Comparison to necropsy findings. Am J Cardiol.
1986; 57(6):450–8. https://doi.org/10.1016/0002-9149(86)90771-x
PMID: 2936235
- De Simone G, Devereux RB, Chinali M, Roman MJ, Lee ET at al.
Metabolic syndrome and left ventricular hypertrophy in the
prediction of cardiovascular events:The Strong Heart Study. Nutr
Metab Cardiovasc Dis. 2009;19(2):98–104.
doi:10.1016/j.numecd.2008.04.001.
- Bastać D. Komparativna studija hipertrofije miokarda
izazvane hipertireozom, esencijalnom hipertenzijom i gojaznošću,
doktorska disertacija,. Medicinski fakultet Univerziteta u
Beogradu. Beograd 1998].
- Sayin BY and Oto A. Left Ventricular Hypertrophy: Etiology-Based
Therapeutic Options.Cardiol Ther. 2022;11(2):203–230. Published
online 2022 Mar 30. doi: 10.1007/s40119-022-00260-y PMCID:
PMC9135932 PMID: 35353354
- Raman S V. The Hypertensive Heart. An Integrated
Understanding Informed by Imaging. J Am Coll Cardiol.
2010;55(2):91–6. 10.1016/j.jacc.2009.07.059
- Messerli FH, Rimoldi SF, Bangalore S. The Transition From
Hypertension to Heart Failure: Contemporary Update. JACC Hear
Fail. 2017;5(8):543–51. 10.1016/j.jchf.2017.04.012
- Díez J, Frohlich ED. A translational approach to
hypertensive heart disease. Hypertension. 2010;55:1–8.
10.1161/HYPERTENSIONAHA.109.141887
- Santos M, Shah AM. Alterations in cardiac structure and
function in hypertension. Curr Hypertens Rep. 2014;16(428):1–10.
- Aurigemma GP, De Simone G, Fitzgibbons TP. Cardiac
remodeling in obesity. Circ Cardiovasc Imaging.
2013;6(1):142–52.
- Mahajan R, Lau DH, Sanders P. Impact of obesity on cardiac
metabolism, fibrosis, and function. Trends Cardiovasc Med.
2015;25(2):119–26.
- Alpert MA, Lavie CJ, Agrawal H, Aggarwal KB, Kumar SA.
Obesity and heart failure: epidemiology, pathophysiology,
clinical manifestations, and management. Transl Res.
2014;164(4):345–56.
- Alpert MA, Lavie CJ, Agrawal H, Kumar A, Kumar SA. Cardiac
Effects of Obesity. J Cardiopulm Rehabil Prev. 2016;36:1–11.
- Lorenzo-Almoros A, Tuñón J, Orejas M, Cortés M, Egido J,
Lorenzo Ó. Diagnostic approaches for diabetic cardiomyopathy.
Cardiovasc Diabetol. 2017;16(28):1–11.
- De Simone G, Mancusi C, Izzo R, Losi MA, Aldo Ferrara L.
Obesity and hypertensive heart disease: focus on body
composition and sex differences. Diabetol Metab Syndr.
2016;8(79):1–9.
- Oktay AA, Lavie CJ, Milani R V., Ventura HO, Gilliland YE,
Shah S, et al. Current Perspectives on Left Ventricular Geometry
in Systemic Hypertension. Prog Cardiovasc Dis.
2016;59(3):235–46.
- Ojji DB, Adebiyi AA, Oladapo OO, Adeleye JA, Aje A, Ogah OS,
et al. Left ventricular geometric patterns in normotensive type
2 diabetic patients in nigeria: An echocardiographic study. Prev
Cardiol. 2009;12(4):184–8.
- Eguchi K, Kario K, Hoshide S, Ishikawa J, Morinari M,
Shimada K. Type 2 diabetes is associated with left ventricular
concentric remodeling in hypertensive patients. Am J Hypertens.
2005;18(1):23–9. 10.1016/j.amjhyper.2004.08.024
- Milani R V., Lavie CJ, Mehra MR, Ventura HO, Kurtz JD,
Messerli FH. Left ventricular geometry and survival in patients
with normal left ventricular ejection fraction. Am J Cardiol.
2006;97(7):959–63. 10.1016/j.amjcard.2005.10.030
- Cuspidi C, Rescaldani M, Sala C, Grassi G. Left-ventricular
hypertrophy and obesity: A systematic review and meta-analysis
of echocardiographic studies. J Hypertens. 2014;32(1):16–25.
10.1097/HJH.0b013e328364fb58
- Cuspidi C, Sala C, Negri F, Mancia G, Morganti A. Prevalence
of left-ventricular hypertrophy in hypertension: An updated
review of echocardiographic studies. J Hum Hypertens.
2012;26(6):343–9. 10.1038/jhh.2011.104
- Wachtell K, Bella JN, Liebson PR, Gerdts E, Dahlöf B, Aalto
T, et al. Impact of different partition values on prevalences of
left ventricular hypertrophy and concentric geometry in a large
hypertensive population: the LIFE study. Hypertension. 2000;35(1
Pt 1):6–12. 10.1161/01.hyp.35.1.6
- Alpert MA, Omran J, Mehra A, Ardhanari S. Impact of Obesity
and Weight Loss on Cardiac Performance and Morphology in Adults.
Prog Cardiovasc Dis. 2014;56(4):391–400.
10.1016/j.pcad.2013.09.003
- Lembo M, Esposito R, Lo Iudice F, Santoro C, Izzo R, De Luca
N, et al. Impact of pulse pressure on left ventricular global
longitudinal strain in normotensive and newly diagnosed,
untreated hypertensive patients. J Hypertens. 2016;1201–7.
10.1097/HJH.0000000000000906
- Drazner MH. The progression of hypertensive heart disease.
Circulation. 2011;123(3):327–34.
10.1161/CIRCULATIONAHA.108.845792
- Bastać D. et al. :Razlike u distribuciji tipa geometrijske
remodelacije u hipertrofiji leve komore izazvane hipertenzijom i
gojaznošću . Zbornik radova IV Kongres Interne medicine
Jugoslavije ,Igalo 30.09.1997.
- Bastać D. et al. Udruženost insulinske rezistencije i
hipertrofije miokarda. Zbornik radova VI Kongres Interne
medicine Jugoslavije, Beograd 2000.
- Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, at
al. International Atherosclerosis Society; International Chair
on Cardiometabolic Risk Working Group on Visceral Obesity.
Visceral and ectopic fat, atherosclerosis, and cardiometabolic
disease: a position statement. Lancet Diabetes Endocrinol.
2019;7(9):715-725. doi: 10.1016/S2213-8587(19)30084-1. Epub 2019
Jul 10. PMID: 31301983.
|
|
|
|