| |
|
|
INTRODUCTION
Acute appendicitis is the most common intra-abdominal surgical
emergency [1]. In Serbia, the morbidity of acute appendicitis is
similar to global trends, and the overall lifetime risk is
approximately 8.6% in men and 6.7% in women [2]. The diagnosis and
management of acute appendicitis can be complex, as they require the
exclusion of various differential diagnoses and prioritization of
surgical intervention according to disease severity. Timely and
accurate treatment remains essential for reducing
appendicitis-related morbidity.
Distinguishing between uncomplicated and complicated appendicitis is
crucial for determining the appropriate therapeutic approach [3].
Inadequate or delayed diagnosis and treatment of complicated
appendicitis are associated with serious complications and
postoperative morbidity, further emphasizing the importance of
identifying parameters that reflect disease severity [4].
Accurate differentiation between these two forms aims to support the
selection of the most appropriate therapy, while simultaneously
reducing the number of unnecessary surgical interventions and the
risk of associated complications. In addition to laparoscopic
appendectomy, which remains the gold standard for the treatment of
complicated appendicitis, a conservative approach is increasingly
being used in the management of uncomplicated cases [5–7].
The diagnosis of appendicitis is primarily based on the clinical
presentation, although inflammatory markers, ultrasound, and
computed tomography can contribute to diagnostic accuracy [8]. In
our institution, ultrasound examination is routinely used together
with the assessment of C-reactive protein (CRP) levels and white
blood cell (WBC) count to facilitate diagnosis and evaluate disease
severity. CT is used rarely, and only in cases where the clinical
presentation and laboratory findings are not sufficiently clear.
C-reactive protein (CRP) is an inflammatory marker that has been
identified in several studies as an independent predictor of
complicated appendicitis [9,10].
The main objective of this study is to determine whether CRP can be
used to distinguish between complicated (gangrenous or perforated)
and uncomplicated appendicitis.
MATERIALS AND METHODS
This study presents a retrospective analysis of 231 patients with
clinical signs of acute appendicitis who were hospitalized at the
Department of General Surgery of the Clinical Hospital Center (KBC)
Zemun between December 2021 and September 2023. All data used in the
study were obtained from medical records. The patients underwent
surgical treatment, either open or laparoscopic appendectomy, and
the diagnosis of acute appendicitis was confirmed by postoperative
histopathological examination of the removed appendix.
Based on clinical, intraoperative, and histopathological findings,
the patients were divided into two groups: those with uncomplicated
appendicitis and those with complicated appendicitis. Uncomplicated
appendicitis was defined as catarrhal or phlegmonous inflammation of
the appendix, whereas complicated appendicitis referred to
gangrenous inflammation, with or without perforation.
In addition to analyzing and comparing C-reactive protein levels,
white blood cell counts, and ultrasound findings, the study also
assessed various clinical and demographic parameters. These included
symptom duration, the presence or absence of febrile episodes, and
the existence of comorbidities. Basic demographic characteristics
such as patient sex and age were also included to evaluate their
potential impact on clinical presentation and disease course. A body
temperature higher than 37.4°C was considered significant.
Every clinical suspicion of appendicitis was further confirmed by
mandatory laboratory analyses and ultrasound examination to increase
diagnostic accuracy and guide further management. A positive
ultrasound finding was established based on the identification of
one or more of the following criteria: presence of free
intraperitoneal fluid, regional lymphadenopathy, and/or an increased
appendiceal diameter with thickening of the appendiceal wall.
Statistical analysis was performed using SPSS software, version 21.
Variables between the two patient groups were compared using the
Mann–Whitney U test for numerical data and the chi-square test for
categorical data. Statistical significance was defined as a p-value
of less than 0.05.
RESULTS
The sample of 231 patients diagnosed with appendicitis during the
study period was divided into two groups. The first group consisted
of 168 patients (72.73%) with uncomplicated appendicitis, while the
second group included 63 patients (27.27%) with complicated
appendicitis. The overall patient population comprised 110 men
(47.62%) and 121 women (52.38%). Among patients with complicated
appendicitis, 34 (54%) were men and 29 (46%) were women, whereas in
the group with uncomplicated appendicitis, 76 (45.2%) were men and
92 (54.8%) were women. No statistically significant difference in
sex distribution was observed between the two groups (p = 0.242).
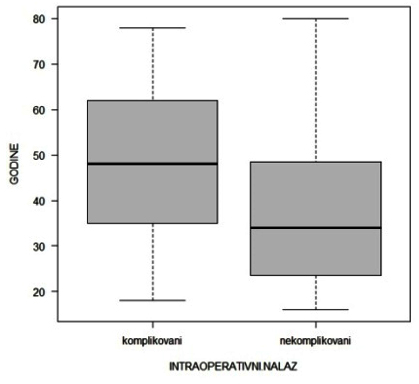
The mean age of our patients was 40.31 ± 17.06 years, with the
youngest patient being 16 and the oldest 80 years old. In the
subgroup of patients with complicated appendicitis, the median age
was 47 years. In contrast, patients with uncomplicated appendicitis
were significantly younger, with a median age of 34 years,
representing a statistically significant difference (p < 0.01).
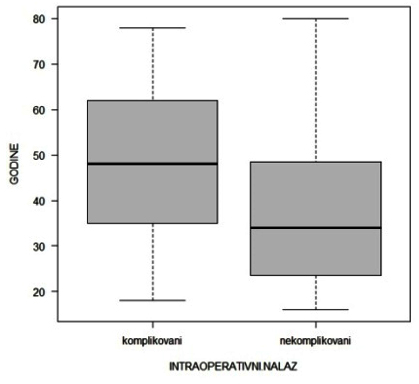
Figure 1. The box-plot diagram illustrates the
relationship between patient age and intraoperative findings in
complicated and uncomplicated appendicitis. The diagram indicates a
statistically significant difference in the severity of
intraoperative findings between younger and older patients. The
central line within each box represents the median age, while the
edges of the box denote the first and third quartiles.
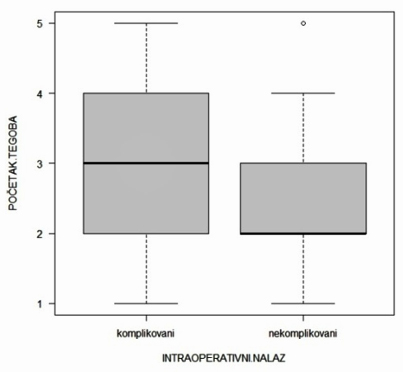
In most patients with complicated inflammation, symptoms appeared
within 24 to 48 hours prior to establishing the preoperative
diagnosis. In contrast, patients with uncomplicated inflammation
most commonly experienced symptoms for less than 24 hours before
arriving at the hospital. This difference in symptom duration
between the two groups was statistically significant (p < 0.01),
indicating an association between longer symptom duration and the
development of complicated disease. These findings highlight the
importance of early clinical assessment and intervention to reduce
the risk of complications.
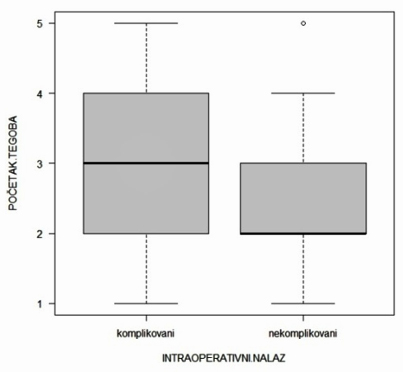
Figure 2. The box-plot diagram illustrates the
relationship between symptom duration and intraoperative findings in
complicated and uncomplicated appendicitis. The diagram shows that
longer symptom duration is associated with a higher incidence of
complicated intraoperative findings. The central line within each
box represents the median duration, while the edges of the box
denote the first and third quartiles.
A total of 63 patients (27.27%) experienced episodes of elevated
body temperature during the course of their symptoms, of whom 26 had
complicated and 37 had uncomplicated appendicitis. Considering the
difference in group size, the difference in the presence of fever
between the groups was statistically significant (p < 0.01).
Regarding comorbidities, a total of 7 patients (3.02%) were
diagnosed with diabetes mellitus. Of these, 5 patients were in the
uncomplicated appendicitis group, while 2 patients were in the
complicated appendicitis group. Statistical analysis did not show a
significant difference in the prevalence of diabetes between the
groups, suggesting that in this sample, the presence of DM did not
significantly influence the likelihood of developing complicated
appendicitis.
Ultrasound examination demonstrated findings indicative of acute
appendicitis in 134 patients (58.01%), while 97 patients (41.99%)
had no ultrasonographic evidence of the disease. Among patients with
positive ultrasound findings, the prevalence of complicated versus
uncomplicated appendicitis was assessed. Although a higher
percentage of patients with positive findings had complicated
appendicitis, the difference between the groups was not
statistically significant (p = 0.134).
In this study, the mean white blood cell count in peripheral blood
was 12.61 × 0**9/L ± 4.64 × 0**9/L, indicating that most patients
presented with leukocytosis. In patients with uncomplicated
appendicitis, leukocyte values ranged from 2.2 × 0**9/L to 25.2 ×
0**9/L, with a mean of 11.8 × 10**9/L. In the complicated
appendicitis group, leukocyte counts ranged from 4.3 × 0**9/L to
27.8 × 0**9/L, with a mean value of 14.4 × 0**9/L. Comparative
analysis of this inflammatory marker between the two groups
demonstrated a statistically significant difference (p < 0.01).
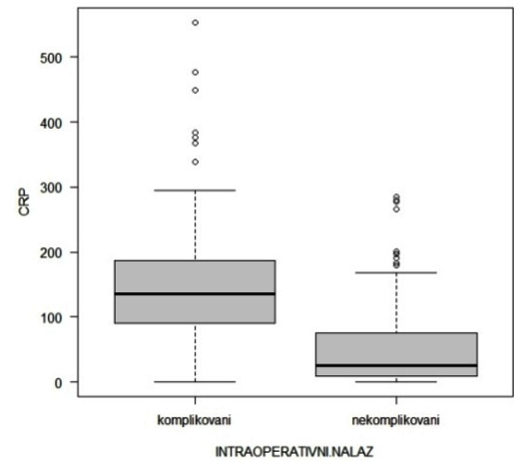
C-reactive protein (CRP) values among patients varied considerably,
with a standard deviation slightly lower than the mean, amounting to
66.62 ± 65.60 mg/L. CRP concentrations ranged from 0.2 mg/L to 265.4
mg/L. The median CRP level in patients with uncomplicated
appendicitis was 24.55 mg/L, which was significantly lower than the
median of 109 mg/L observed in patients with complicated
appendicitis.
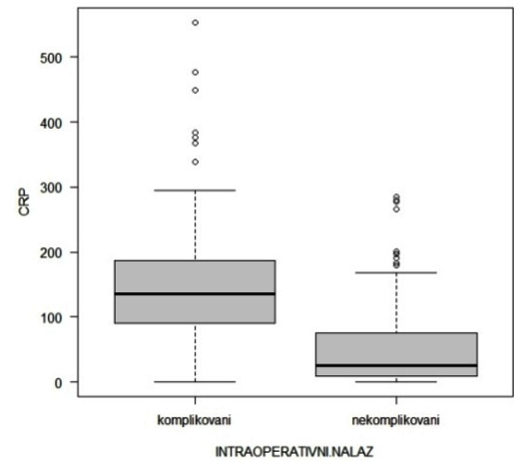
Figure 3. The box-plot diagram illustrates the
relationship between C-reactive protein (CRP) levels and
intraoperative findings in appendicitis. Higher CRP levels are
associated with more severe, complicated forms of appendicitis. The
central line within each box represents the median CRP value, while
the edges of the box denote the first and third quartiles.
DISCUSSION
Preoperative differentiation between complicated and
uncomplicated acute appendicitis remains a major clinical challenge,
particularly when clinical findings are unclear and laboratory tests
lack sufficient specificity [11,12]. This diagnostic uncertainty
contributes to a substantial rate of misdiagnosis, which, according
to several studies, ranges between 12% and 30% [2,8,10]. Such errors
may lead to unnecessary surgical intervention or delays in
treatment, thereby worsening clinical outcomes. Therefore, improving
diagnostic tools and criteria is essential for optimizing disease
management and reducing negative appendectomies and complications.
Traditionally, early appendectomy has been recommended for
uncomplicated appendicitis to prevent rupture [13]. However, recent
randomized studies [13–15] and meta-analyses [16,17] show that
nonoperative antibiotic treatment may be successful in carefully
selected patients with uncomplicated appendicitis. According to the
updated guidelines of the World Society of Emergency Surgery (WSES),
established at the Jerusalem Consensus Conference in 2020,
antibiotic therapy is recommended as a safe and effective
alternative to surgery in patients with uncomplicated appendicitis
without appendicolithiasis. It is important to note that
unrecognized perforation may lead to severe complications such as
abscess formation and purulent peritonitis [19]. The reported
perforation rate in acute appendicitis ranges between 20% and 34%
[20–22]. Among patients treated nonoperatively, it should be
emphasized that there is an approximately 39% risk of recurrence
within 5 years [14,18].
Laparoscopic appendectomy remains the gold standard for the
management of suspected complicated appendicitis [23]. The need for
a more invasive approach is justified by the serious complications
that may arise, including infection, ileus, intra-abdominal abscess,
and fistula formation [24–26]. Delaying surgery increases the risk
of life-threatening conditions and rehospitalization [27].
Demographic characteristics, particularly age and sex, have been
identified as significant factors in the development of complicated
appendicitis. Birben et al. reported a higher incidence of
complicated appendicitis in older and male patients [28]. Our study
did not demonstrate a statistically significant sex difference, but
patients with complicated appendicitis were significantly older.
This may be explained by age-related declines in immune function and
physiological reserves. Numerous studies report similar findings
[2,3,6,29,30].
A long interval between symptom onset and diagnosis is directly
associated with the development of complications. Our study confirms
that longer symptom duration is a predictor of complicated disease,
consistent with previous research [2,3,8,23,30,31].
Elevated temperature (≥37.4°C) has been shown to be a clinically
useful indicator of complicated appendicitis [30,31,33]. Our
findings, as well as the study by Akai et al. [34], confirm the
significance of body temperature in assessing disease severity.
Although diabetes is associated with immune dysfunction and a more
severe course of appendicitis, our study did not show a significant
association, likely due to the small number of diabetic patients and
better disease control in our institution [2,35].
Ultrasound is frequently the first diagnostic modality, but it is
limited by subjective interpretation and patient-related factors
[3,36,37]. Our results confirm that ultrasound alone is insufficient
for distinguishing complicated from uncomplicated disease and should
be used in combination with clinical evaluation and laboratory
markers.
Leukocytosis is an important but nonspecific marker. Our results
confirm its correlation with complicated appendicitis, although it
lacks sufficient standalone predictive value [4,7,8,27,38].
CRP, as an acute-phase protein, exhibits proportional increases with
the severity of inflammation [3,27,29,30,31,33,38,39]. Our study
confirmed its markedly elevated levels in complicated cases (median
109 mg/L), further supporting its diagnostic utility.
CONCLUSION
Our study confirms that older age, elevated body temperature, longer
symptom duration, and increased CRP levels are key factors
associated with complicated acute appendicitis. CRP emerged as the
most reliable preoperative biomarker for assessing disease severity.
These findings emphasize the need to integrate clinical evaluation
with selected laboratory parameters, particularly CRP, to ensure a
more accurate preoperative diagnosis and the implementation of
timely therapeutic strategies.
LITERATURE:
- Sartelli M, Catena F, Ansaloni L, Coccolini F, Corbella D,
Moore EE, et al. Complicated intra-abdominal infections
worldwide: the definitive data of the CIAOW study. World J Emerg
Surg. 2014;9:37. doi:10.1186/1749-7922-9-37. PMID:24883079.
- Naderan M, Babaki AES, Shoar S, Mahmoodzadeh H, Nasiri S,
Khorgami Z. Risk factors for the development of complicated
appendicitis in adults. Turk J Surg. 2016;32(1):37-42.
doi:10.5152/UCD.2015.3031.
- Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J,
Boermeester MA. Scoring system to distinguish uncomplicated from
complicated acute appendicitis. Br J Surg. 2015;102(8):979-90.
doi:10.1002/bjs.9835. PMID:25963411.
- Kaminskas ĄA, Lukšaitė-Lukštė R, Jasiūnas E, Samuilis A,
Augustinavičius V, Kryžauskas M, et al. The dynamics of
inflammatory markers in patients with suspected acute
appendicitis. Medicina (Kaunas). 2021;57(12).
doi:10.3390/medicina57121384. PMID:34946329.
- Coccolini F, Fugazzola P, Sartelli M, Cicuttin E, Sibilla
MG, Leandro G, et al. Conservative treatment of acute
appendicitis. Acta Biomed. 2018;89(9-S):119-34.
doi:10.23750/abm.v89i9-s.7905. PMID:30561405.
- Hiroi S, Hamaoka M, Miguchi M, Misumi T, Yamamoto Y, Ikeda
S, et al. Comparison of three clinical trials of preoperative
predictors for complicated appendicitis. In Vivo.
2022;36(5):2442. doi:10.21873/invivo.12978. PMID:36099130.
- Bom WJ, Scheijmans JCG, Salminen P, Boermeester MA.
Diagnosis of uncomplicated and complicated appendicitis in
adults. Scand J Surg. 2021;110(2):170-9.
doi:10.1177/14574969211008330. PMID:33851877.
- Ribeiro AM, Romero I, Pereira CC, Soares F, Gonçalves Á,
Costa S, et al. Inflammatory parameters as predictive factors
for complicated appendicitis: a retrospective cohort study. Ann
Med Surg (Lond). 2022;74:103266. doi:10.1016/j.amsu.2022.103266.
- Kim M, Kim SJ, Cho HJ. International normalized ratio and
serum C-reactive protein are feasible markers to predict
complicated appendicitis. World J Emerg Surg. 2016;11:1.
doi:10.1186/s13017-016-0081-6.
- Uludağ SS, Akıncı O, Güreş N, Tunç E, Erginöz E, Şanlı AN,
et al. Effectiveness of pre-operative routine blood tests in
predicting complicated acute appendicitis. Ulus Travma Acil
Cerrahi Derg. 2022;28(11):1590-6. doi:10.14744/tjtes.2021.13472.
PMID:36282156.
- Kim HY, Park JH, Lee YJ, Lee SS, Jeon JJ, Lee KH. Systematic
review and meta-analysis of CT features for differentiating
complicated and uncomplicated appendicitis. Radiology.
2018;287(1):104-15. doi:10.1148/radiol.2017171260.
PMID:29173071.
- Rait JS, Ajzajian J, McGillicuddy J, Sharma A, Andrews B.
Acute appendicitis and the role of pre-operative imaging: a
cohort study. Ann Med Surg (Lond). 2020;59:258-63.
doi:10.1016/j.amsu.2020.10.008.
- Andersson RE. The natural history and traditional management
of appendicitis revisited: spontaneous resolution and
predominance of prehospital perforations imply that a correct
diagnosis is more important than an early diagnosis. World J
Surg. 2007;31(1):86-92. doi:10.1007/s00268-006-0056-y.
PMID:17180556.
- Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M,
Rantanen T, et al. Antibiotic therapy vs appendectomy for
treatment of uncomplicated acute appendicitis: the APPAC
randomized clinical trial. JAMA. 2015;313(23):2340-8.
doi:10.1001/jama.2015.6154. PMID:26080338.
- Park HC, Kim MJ, Lee BH. Randomized clinical trial of
antibiotic therapy for uncomplicated appendicitis. Br J Surg.
2017;104(13):1785-90. doi:10.1002/bjs.10660. PMID:28925502.
- Yang Z, Sun F, Ai S, Wang J, Guan W, Liu S. Meta-analysis of
studies comparing conservative treatment with antibiotics and
appendectomy for acute appendicitis in the adult. BMC Surg.
2019;19(1):90. doi:10.1186/s12893-019-0578-5. PMID:31412833.
- Prechal D, Damirov F, Grilli M, Ronellenfitsch U. Antibiotic
therapy for acute uncomplicated appendicitis: a systematic
review and meta-analysis. Int J Colorectal Dis.
2019;34(6):963-71. doi:10.1007/s00384-019-03296-0.
PMID:31004210.
- Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G,
Gori A, et al. Diagnosis and treatment of acute appendicitis:
2020 update of the WSES Jerusalem guidelines. World J Emerg
Surg. 2020;15:27. doi:10.1186/s13017-020-00306-3. PMID:32295644.
- Horn CB, Tian D, Bochicchio GV, Turnbull IR. Incidence,
demographics, and outcomes of nonoperative management of
appendicitis in the United States. J Surg Res. 2018;223:251-8.
doi:10.1016/j.jss.2017.10.007. PMID:29198605.
- Cueto J, D’Allemagne B, Vázquez-Frias JA, Gomez S, Delgado
F, Trullenque L, et al. Morbidity of laparoscopic surgery for
complicated appendicitis: an international study. Surg Endosc.
2006;20(5):717-20. doi:10.1007/s00464-005-0402-4. PMID:16544077.
- Khan MS, Siddiqui MTH, Shahzad N, Haider A, Chaudhry MBH,
Alvi R. Factors associated with complicated appendicitis: view
from a low-middle income country. Cureus. 2019;11(5):e4765.
doi:10.7759/cureus.4765. PMID:31363446.
- Patel SV, Nanji S, Brogly SB, Lajkosz K, Groome PA, Merchant
S. High complication rate among patients undergoing appendectomy
in Ontario: a population-based retrospective cohort study. Can J
Surg. 2018;61(6):412-7. doi:10.1503/cjs.011517. PMID:30265637.
- Bancke Laverde BL, Maak M, Langheinrich M, Kersting S, Denz
A, Krautz C, et al. Risk factors for postoperative morbidity,
prolonged length of stay and hospital readmission after
appendectomy for acute appendicitis. Eur J Trauma Emerg Surg.
2023;49(3):1355-66. doi:10.1007/s00068-023-02225-9.
PMID:36708422.
- Moreira LF, Garbin HI, Da-Natividade GR, Silveira BV, Xavier
TV. Predicting factors of postoperative complications in
appendectomies. Rev Col Bras Cir. 2018;45(5):e1920.
doi:10.1590/0100-6991e-20181920. PMID:30462825.
- Skjold-Ødegaard B, Søreide K. The diagnostic differentiation
challenge in acute appendicitis: how to distinguish between
uncomplicated and complicated appendicitis in adults.
Diagnostics (Basel). 2022;12(7):1724.
doi:10.3390/diagnostics12071724. PMID:35885627.
- Wu T, Yang Y, Wu Y, Lu L, Dong S. Complications after
appendectomy in patients with treated appendicitis: results from
a retrospective study. Ann Palliat Med. 2021;10(12):12546-53.
doi:10.21037/apm-21-3295. PMID:35016452.
- Binboga S, Isiksacan N, Binboga E, Kasapoglu P, Surek A,
Karabulut M. Diagnostic value of serum cytokines in predicting a
complicated acute appendicitis. An Acad Bras Cienc.
2022;94(2):e20201947. doi:10.1590/0001-3765202220201947.
PMID:35507979.
- Birben B, Sönmez BM, Er S, Özden S, Kösa MT, Tez M. External
validation of the appendistattm score and comparison with CRP
levels for the prediction of complicated appendicitis. Ulus
Travma Acil Cerrahi Derg. 2021;27(2):187-91.
doi:10.14744/tjtes.2020.68246. PMID:33630294.
- Kang CB, Li WQ, Zheng JW, Li XW, Lin DP, Chen XF, et al.
Preoperative assessment of complicated appendicitis through
stress reaction and clinical manifestations. Medicine
(Baltimore). 2019;98(23):e15768.
doi:10.1097/MD.0000000000015768. PMID:31169674.
- Fujiwara K, Abe A, Masatsugu T, Hirano T, Hiraka K, Sada M.
Usefulness of several factors and clinical scoring models in
preoperative diagnosis of complicated appendicitis. PLoS One.
2021;16(7):e0255253. doi:10.1371/journal.pone.0255253.
PMID:34314464.
- Sasaki Y, Komatsu F, Kashima N, Suzuki T, Takemoto I, Kijima
S, et al. Clinical prediction of complicated appendicitis: a
case-control study utilizing logistic regression. World J Clin
Cases. 2020;8(11):2127-36. doi:10.12998/wjcc.v8.i11.2127.
- Peeters T, Martens S, D’Onofrio V, Stappers MHT, van der
Hilst JCH, Houben B, et al. An observational study of innate
immune responses in patients with acute appendicitis. Sci Rep.
2020;10(1):13530. doi:10.1038/s41598-020-73798-3. PMID:33060696.
- Imaoka Y, Itamoto T, Takakura Y, Suzuki T, Ikeda S,
Urushihara T. Validity of predictive factors of acute
complicated appendicitis. World J Emerg Surg. 2016;11:21.
doi:10.1186/s13017-016-0107-0. PMID:27708690.
- Akai M, Iwakawa K, Yasui Y, Yoshida Y, Kato T, Kitada K, et
al. Hyperbilirubinemia as a predictor of severity of acute
appendicitis. J Int Med Res. 2019;47(8):3663-9.
doi:10.1177/0300060519856155. PMID:31238753.
- de León-Ballesteros GP, Pérez-Soto R, Zúñiga-Posselt K,
Velázquez-Fernández D. Presentación clínica de la apendicitis
aguda en pacientes inmunocomprometidos por diabetes o VIH/sida.
Gac Med Mex. 2018;154(4):473-9. doi:10.24875/gmm.17003839.
PMID:30250334.
- Karul M, Berliner C, Keller S, Tsui TY, Yamamura J. Imaging
of appendicitis in adults. Rofo. 2014;186(6):551-8.
doi:10.1055/s-0034-1366074. PMID:24760428.
- Bolmers MDM, Bom WJ, Scheijmans JCG, van Geloven AAW,
Boermeester MA, Bemelman WA, et al. Accuracy of imaging in
discriminating complicated from uncomplicated appendicitis in
daily clinical practice. Int J Colorectal Dis.
2022;37(6):1385-91. doi:10.1007/s00384-022-04173-z.
PMID:35583564.
- Patmano M, Çetin DA, Gümüş T. Laboratory markers used in the
prediction of perforation in acute appendicitis. Ulus Travma
Acil Cerrahi Derg. 2022;28(7):960-6.
doi:10.14744/tjtes.2021.83364. PMID:35775680.
- Xu T, Zhang Q, Zhao H, Meng Y, Wang F, Li Y, et al. A risk
score system for predicting complicated appendicitis and aid
decision-making for antibiotic therapy in acute appendicitis.
Ann Palliat Med. 2021;10(6):6133-44. doi:10.21037/apm-21-26.
PMID:34118840.
|
|
|
|