| |
INTRODUCTION
A large number of approved medicines by official pharmacopoeia as
well as alternative healing medicines and herbal medicines, could
provoke toxic hepatitis. Lately, a term ‘herbal related toxic hepatitis’
has appeared in literature because there are more and more cases of
toxic liver damage caused by the use of herbal medicines and their
preparations and final medicines based on plants [1]. However, it is
considered in everyday practice that those medicines could not provoke
harmful effects and we recognize them very rarely as etiological factors
of many unexplained cases of liver damage. For these reasons, but also
due to the fact that patients sometimes take many medicines at the same
time, diagnosis setting on herbal hepatotoxity could be very difficult.
According to the type of lesions provoked by herbal medicines, there are
parenchymic and cholestasic forms of hepatitis. There, the agents with
toxic effect cause, first of all, parenchymic damage, and those ones
with hypersensitive effect the cholestasic form of hepatitis. It is
possible that the same agent has effect in two ways [2]. Hepatotoxic
substances or their metabolites damage hepatocytes directly resulting
into necrosis or damage the cell integrity such as by provoking
“self-destruction” that is programmed cell death apoptosis [3].
The liver has great importance in the metabolism of medicines including
herbal medicines, and hepatocytes are exposed to concentrations of
newly-formed metabolites that are formed in reactions of medicine
oxidation with participation of cytochrome P450 enzyme. Chemically
reactive metabolites could form incovalent bonds with the aimed
molecules or change the aimed molecule by covalent interactions, and
both reactions are possible at the same time. Potential cytotoxic
incovalent reactions are lipid peroxidation, generation of toxic
radicals, discharging of glutathione level, modification of sulphydril
groups. Lipid peroxidation of polysaturated fats could be started by
reactive metabolite or reactive oxygen radicals formed by such
metabolites. Lipid peroxiradicals by chain reaction over peroxide
cascade include much more lipids in membrane and provoke cell damage and
finally its death. If protective mechanisms, as well as glutathione
peroxidase and vitamin E, are not included enough and on time, lipid
peroxidation will not be enough to result into cell necrosis. But
generation of toxic cell radicals could result into cytotoxicity. Toxic
radicals are formed by reduction of molecular oxygen to superoxide
anions, and then by enzymic conversion to hydrogen peroxide or reactive
free radicals as well as hydroperoxide and hydroxyl radicals and the so
called singlet oxygen. Those reactive oxygen radicals are cytotoxic over
lipid peroxidation, too. “Oxidative stress” is formed by reactions that
cause depletion of glutathione level, which is the result of balance
disturbance between peroxidants and antioxidants in cells in favour of
prooxidant conditions. Oxidoreductive cycle of glutathione (GSH) that is
normally in a couple with glutathione disulphide (GSSG), presents a
protective mechanism that decreases damage of cells due to oxidative
stress. Free oxygen radicals transform GSH into GSSG (where GSH is
regenerated under the influence of GSSG reductase with activity
depending on NAADPH). If a drop of GSSH level appears for 20 – 30%, the
defensive cell system will be disturbed and a death of cell can appear.
Modification of sulphydril groups could be formed by action of free
oxygen radicals that change reversibly sulphydril group or covalent
interaction. Free sulphydril group has a crucial importance for
catalytic activity of many enzymes, and their modification results into
inactivation of enzymes. Inactivation of enzymes results into increased
Ca concentration of cell, which causes the death of cell.
Covalent interactions result into changes on proteins to become
immunogenous, and DNK changes result into mutagenes responsible for
carcinogenesis and teratogenesis [2].
For treatment of cholecystolithiasis, people use medicaments for
gallstone ejecting and melting. For the aim of gallstone melting in the
bile duct, the medicaments based on black radish juice and in
combination with other plants or “healing” medicines are very favorable.
Therefore, black radish in a large number of handbooks and instructions
in the field of phytotherapy, homeopathy and self-treatment is a very
powerful hepatoprotective and well-known healing medicine in the
treatment of liver disorders and bile ducts. There are a large number of
internet sites on healing effects of black radish on liver and bile
ducts, and there are also a number of forums on the topic: “Does black
radish melt gallstones in bile ducts?”
Also, in medical expert literature, the black radish juice has proved
antioxidant features, although the mechanism of biological active
components of black radish on lipid peroxidation is not completely clear
[5]. It was established that the black radish extract decreases the
level of lipid peroxidation and this effect depends on juice
concentration [6]. It was shown that antiflamatory and antiapoptosic
features of black radish have a hepatoprotective activity.
In an experiment with rabbits with cadmium (Cd) provoked liver damage, a
significant decrease of the total level of liver bilirubins and enzymes
resulted in rabbits fed with powder of dried black radish [7]. The
effect of black radish root is also favourable on the structure and
redox system status of colon mucosa of mice. After a rich fat diet, the
mice had inflammation and lesion of enetrocyte. After nutrition with
black radish granulates, the results were similar as the ones with mice
in the control group that were on balanced nutrition. The colon mucosa
was better – the cells like cup were increased and inflammation was
removed [8]. In recommendation for diet in prevention of carcinoma of
gall bladder, the use of black radish decreases significantly the risk
for this organ carcinoma [9], which is possible due to the fact that one
isocyanate-sulphoraphen, isolated from black radish “in vitro” shows the
activity of mutagenous inhibition [10].
Black radish belongs to the order of cruciferous plants. It is consider
that the origin of this plant is in Asia and there are some assumptions
that it originated from a wild radish. Nowadays there is no wild radish
in nature. It is known that the ancient Egyptians made oil from wild
radish seed. In the ancient Greek and Roman, the healing characteristics
of radish were known also in treatment of respiratory organs. The radish
was mentioned in France during the renaissance period, when the effect
of black radish was specially used for bile secretion [11]. This rooty
plant in a form of beet has black surface and white fleshy root. It has
extremely hot taste. When it is used in raw condition, it usually causes
flatulence in the stomach. Black radish is not mainly used as nutrient,
but as addition to food (mainly salads) or as a diet-healing ingredient
of food. It is reach with C vitamin and has antioxidative
characteristics. As regards minerals, it is reach in potassium. Due to
the content of many plant fibres and certainly also water – that
increases the transit of stool through the intestine, it is recommended
in nutrition of patients with constipation. It is considered that some
ingredients of black radish improve discharging of gall bladder and bile
vessels and therefore it is recommended in common medicine to the
patients with hepatobilliary system diseases. Due to antibacterial
effects, it is also used by patients with disorders of intestinal flora.
Ethereal oils of black radish are secreted over mucosa of the
respiratory system, so this plant is also used in the treatment of cough
[12].
CASE REPORT
Thirty year-old patient Z.G. from Podgorica. For a couple of last
years she knows about having the stones in the bile duct. She has
periodically the undetermined pains under the right rib arch. She has
heard from friends that black radish is efficient in melting of bile
stones and starts “a therapy with black radish juice”.
She drinks 150 ml of black radish juice two times every day. She
squeezes juice in a juicer and for daily dose of 300 ml juice, she mills
and squeezes about 900 gr of raw black radish. The juice has a repulsive
extremely hot taste and unpleasant smell. Upon consumption of each dose
she has burning in the stomach and indescribable feeling of nausea
followed with shaking and perspiration as well as frequent mushy stools.
The patient continues persistently with taking of juice thinking that
“it should be” and that it is exactly “the healing effect” of juice.
When, after a month and a half of medicament application she has spent a
sack of 50 kg of black radish, she herself requires a control of
laboratory parameters due to nausea and burning in the stomach, the
personnel in the laboratory checks twice the level of liver enzymes
because they are surprised with the high level of AST (710) and ALT
(1130).
The patient reports for medical examination on 17.03.2007. At the
acceptance, she is afebrile, eupnoic, anirectal cardiopulmonal
compensated. Physical findings of the lungs and the heart are normal. TA
115/70. The stomach is palpatory painful sensitive under the right rib
arch. The liver is palpitated on the edge d.r.1 at deep expirium. The
spleen is not touchable. Pathological resitencies are not palpitated.
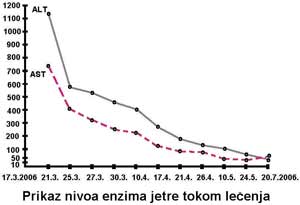
We present Table 1 with the values of enzymes per dates.
All the other laboratory findings, including red and white blood
picture, bilirubins, alkaline phosphatase, gamma GT, fibrinogen,
electrolytes, Fe, glycaemia and lipid status, are many times controlled
and they are always within the limits of reference values.
Markers for viral hepatitis A, B and HIV are negative. ECHO of the upper
abdomen:
Gall bladder with thickened wall, partially filled lumen with a large
number of concrements, diameter up to 8 mm. Liver, spleen, pancreas and
kidneys without noticeable echonoscopic changes.
Esophagogastroduodenoscopy: duodenogastritic biliary reflux without
noticeable changes at the level of mucosa.
Colonoscopy: normal endoscopic findings.
CT of abdomen shows lightly diffuse swollen liver and normal other solid
organs.
We advise hospitalization to the patient which she refuses due to the
family reasons and we conduct medical treatment in home conditions. That
means immediate interruption of the “therapy” with black radish. We
determine a peroral diet to the patient without animal fat, reached with
vitamins and we practice the supported therapy with amino acid infusion
solutions (Amino and Hepasteril). After 10 days, we exclude the infusion
solutions and we peroraly add the amino acid drugs (Essentiale), and
when the enzymes are normalized, we exclude every form of medical
therapy. The patient is under everyday medical supervision, and the
laboratory analyses are controlled every 2-3 days at the beginning and
later rarely. Subjective discomforts have been removed after only two
days of interruption of taking the black radish juice, and laboratory
analyses show gradually continuous decrease of liver enzyme level. We
also control the other biochemical parameters that are not over the
normal values during the treatment. After interruption of medical
therapy, the patient is still on a diet without animal fat. After two
months, liver enzyme levels are completely normalised.
Table 1 presents a review of liver enzyme levels per dates. Figurative
presentation of the data is also presented in Graph 1 in the attachment.
TABLE 1 Review of enzymes per dates |
|
| |
DISCUSSION
A number of herbal drugs were described that could result in enormous
increase of liver enzymes such as noni [13], coffea-coffea, gingseng,
ehinacea, ginkgo biloba, centarium umbellatum.
It was shown that many herbal drugs, mainly from the assortment of
Chinese traditional medicine, Japanese kampo medicine and Indian
ajurveda medicine could cause liver lesions [14, 15].
Hepatotoxic effect of herbal drugs is caused by the effect of various
toxic substances or drug overdosing or combination with other (un)toxic
substances [16].
Contrary to the widespread belief that herbal drugs are a priori safe
and not dangerous, we have presented the case of severe toxic hepatitis
provoked by the use of wider herbal drug that is an excellent
hepatoprotective.
As we have not found any described examples of distinctive hepatotoxity
of black radish in literature and data sources, we think that is
interesting to present such a case.
CONCLUSION
This work presents toxic hepatitis provoked by the use of squeezed
black radish. Black radish is considered as one of the best
hepatotprotectives in folk medicine and phytotherapy, and it was the use
of squeezed black radish that resulted into severe toxic hepatitis.
Again, the validity of famous Paracelsus declaration is confirmed:
“Nihil venenum est et omnia venenum; quod interest portio est” (“Nothing
is poison and everything is poison; the difference is in dosage”).
Interruption of the “therapy”, diet and usage of infusion of amino acid
solutions had a more favourable result. After two months, there is a
completely normalised liver function (restitutio ad integrum).
Although it looks anachronous, it can be concluded that it is still
necessary to work on the increase of health culture of people and
similar incidents could thus be avoided.
REFERENCES
- Haller A C et al., Making a diagnosis of herbal-related toxic
hepatitis West J Med. 2002 January; 176(1): 39–44.
- S.Stefanović Specijalna klinička fiziologija –Medicinska knjiga
beograd-Zagreb 1980 str.437-9
- Braunwald E et al Harrisonova načela interne medicine 15.izdanje
knjiga 2 Bard Fin Beograd & Romanov Banja Luka 2004 ,1737- 42
- Humprey P. Rang et al. Farmakologija 5 izdanje-Prvo srpsko
izdanje Data Beograd 2005, 724-8
- Lugasi A et al. Antioxidant effect of squeezed juice from black
radish (Raphanus sativus L. var niger) in alimentary hyperlipidaemia
in rats Phytotherapy Research Volume 19, Issue 7 , Pages 587 – 591
- Popovic M.et al., Effects of black radish (Raphanus sativus L.)
juice on lipid peroxidation and production of radicals in liposomes
www.prague2003.fsu.edu/content/pdf/248.pdf
- Rifat-uz-Zaman, M. Ahmad Evaluation of Hepatoprotective Effects
of Raphanas sativus L. Journal of Biological Sciences 4 (4):
463-469, 2004
- Sipos P, Hagymasi K et al. Effects of black radish root (Raphanus
sativus L. var niger) on the colon mucosa in rats fed a fat rich
diet. : Phytother Res. 2002 Nov;16(7):677-9.
- Pandey M, Shukla VK.Diet and gallbladder cancer: a case-control
study. : Eur J Cancer Prev. 2002 Aug;11(4):365-8.
- Shishu, Singla AK, Kaur IP.Inhibition of mutagenicity of
food-derived heterocyclic amines by sulphoraphene--an isothiocyanate
isolated from radish. Planta Med. 2003 Feb;69(2):184-6.
-
http://www.zzjzpgz.hr/nzl/14/rotkvica.htm .
-
http://www.dietobio.com/aliments/en/radish.html
- Vanessa Stadlbauer V et al. Hepatotoxicity of NONI juice: Report
of two cases R World J Gastroenterol 2005 August 14;11(30):4758-4760
- Dasgupta A, Review of Abnormal Laboratory Test Results and Toxic
Effects Due to Use of Herbal Medicines Am J Clin Pathol
120(1):127-137, 2003,
- Joseph I.et al. Safety Issues with Herbal Medicine, From
pharmacotherapy
http://www.medscape.com/viewpublication/132
- Richard J. Ko, Perspective on the Adverse Reactions from
Traditional Chinese Medicines , J Chin Med Assoc 2004;67:109-116
|
|