| |
|
|
Epidemiology of Cardiovascular Diseases
Cardiovascular diseases present the number one cause of death
worldwide. WHO estimates that 17.3 million people die from CVDs and
predicted mortality rate by 2030 is more than 23 million people. It
is estimated that 30% of all deaths are due to CVDs. Despite the
trend of lower mortality rate due to CVDs last years, they are still
the main cause of mortality. Burden of CVDs is even more pronounced
in low- and middle-income countries, which account for 80% of all
CVD caused deaths world-wide [1].
Every other person in Croatia, Montenegro and Serbia die from CVDs;
countries are in the group of countries having high risk of CVD
mortality [2, 3, 5]. In Croatia, 48.7% of deaths were due to CVDs in
2011 [2], in Montenegro 56.8% of deaths were due to CVDs in 2006
[3], while in the Republic of Serbia 56.0% of deaths were due to
CVDs in 2007 [4].
National health survey conducted in Mon-tenegro in 2008 showed that
42.8% of adults were diagnosed with chronic disease and the leading
diagnoses were the following: hypertension, hyperlipidemias, and
chronic heart disease [3]. Data from Serbian 2006 study titled
„Health of population in Serbia” shows improvement compared to 2000;
however, RFs for CVDs are still highly abundant. Those data shows
that 33.6% of adults smoke, 46.5% of adults has hypertension, 18.3%
of adults are obese, and 74.3% of the population is physical
inactive [4].
Cardiovascular Diseases Risk Factors
Individual and complex approach to each patient with CVD is
necessary due to the multiple risk factors (RFs) behind CVDs.
Frequently mentioned CVD RFs are listed in the Table 1. RFs like
gender, age, physical build or race cannot be changed. However, the
list of those that can be modified is longer, and through their
modification a direct impact can be made on the development and,
more importantly, prevention of CVDs.
CVD risk assessment is simplified with a wide range of different
risk calculators shown graphically in form of charts that have been
developed to ease up the use by healthcare professionals and
individuals [6, 8]. One of the most known and frequently used is the
chart developed by the World Health Organization (WHO) and the
International Society for Hypertension (ISH) [6]. This tool signals
10 year risk for fatal or non-fatal outcome by including the
following RFs: gender, age, smoking, and cholesterol. In addition,
this prediction is specially adapted for patients with type 2
diabetes; one of the most important systemic disorders linked to
CVDs [9]. On the other hand, some of the newly accepted RFs like
endothelial inflammation, blood clothing, change in lipid profile
after meal, oxidative stress or endothelial function are still not
included in these CVD risk assessment tools.
Table 1. CVDs Risk Factors [6, 7]
| RISK FACTORS THAT CANNOT BE MODIFIED |
Gender
Age
Genetic predisposition
Physical build
Race |
| RISK FACTORS THAT CAN BE MODIFIED |
Smoking (passive smoking)
Low physical activity
Alcohol consumption
Diet
Obesity
Hypertension, diabetes, hyperlipidemia
Stress |
It is believed that physical inactivity contributes to CVD
etiology with 37%. Regular physical activity reduces heart and
coronary disease risk, lowers blood pressure, contributes to body
mass maintenance, has beneficial effect on the psychological and
physical condition of a patient and helps to overcome stress [6, 7,
10]. Thus, importance of physical activity is multifold and in many
ways helps cardiovascular system, for example, increased oxygen
transport to heart muscle increases functionality and electrical
stability of the heart. In addition, physical activity has positive
effect on lipid metabolism, increases HDL cholesterol and decreases
LDL cholesterol, lowers blood pressure, reduces the occurrence of
type 2diabetes, increases insulin sensitivity and reduces
thrombocyte aggregation [10, 11]. Studies have shown that minimum an
hour of jogging per week can reduce the risk of heart disease by
42%, while 30 minutes of brisk walking a day can reduce the risk of
heart disease by about 18% and the risk of stroke by about 11% [12].
Furthermore, 30 minute walking per day is enlisted in the official
preventive guidelines for CVDs [6, 7].
Increased body mass is linked to increased blood lipids,
susceptibility to diabetes and increased blood pressure. Increased
body mass is frequently linked with low physical activity [10]. It
is believed that obesity contributes to CVD etiology with 6%. In
addition, waste circumference over 88 cm for fe-males or over 102 cm
for males is an additional CVD RF [6, 7].
Hypertension (blood pressure >140/90 mmHg) contributes to the
development of CVD by 13%. Currently, 15-37% of the adult population
worldwide has high blood pressure, while at 60 years of age this
prevalence increases to 50% of population. WHO estimates show that
45% of CVD caused deaths are associated with hypertension [13].
Moreover, WHO estimates demonstrate that 6 million people annually
die from the effects of smoking. From that number 600,000 deaths are
due to the effects of passive smoking [14]. The contribution of
smoking is 19%.
In addition, chronic emotional conditions such as stress, anxiety,
hostility, insecurity and depression are taking an increasing toll
on human health. It is believed that the risk from psychological and
social factors for developing CVD is as high as the risk from common
CVD RFs like obesity, smoking and high blood pressure [6, 10].
Studies have shown that men have a higher risk of developing CVD
than women during their childbearing age. This effect is attributed
to protecting effect of hormones. After menopause, the incidence of
coronary heart disease in men and women gradually equalizes. After
60 years of age, this ratio is 1:1. According to statistics, women
have fever CVDs diagnosed, but if they are diagnosed with any of
CVDs they die more often [6, 7, 15]. This trend was confirmed for
Croatia [2]. However, it is important to stress that both men and
premenopausal women respond positively in lipid profile and blood
pressure after introduction of the diet for people with
cardiovascular risk [16].
Furthermore, with aging human body gets more exposed to the
environment, which results in more frequent complications; heart and
blood vessels are no exception. Risk for coronary heart disease is
higher in men over age 40 and for women over age 50, especially if
they are exposed to two or more RFs [7, 10].
Some studies indicate that the tendency towards CVDs is inherited.
It is not a classical hereditary transmission of the disease; it is
more a clear correlation between the disease in parents and
manifestation in children [10].
Nutritional Treatment of Patients Diagnosed with Cardiovascular
Disease
or Risk Factors
Treating a patient with cardiovascular dis-ease (CVD) diagnosis
is very complex and it has to be individualized, and treatment
always includes change of their diet [17, 18]. Frequently, these
patients are prescribed a hypocaloric diet. If the first stage did
not result in significant change of blood parameters (usually total
cholesterol and LDL cholesterol), statins are introduced. Statins
have proven their beneficial effect in lowering LDL cholesterol and
consequently reducing cardiovascular events incidence [19].
Dietary Guidelines
It should be pointed out that the need for change in diet in
terms of preventing chronic noncommunicable diseases was acknowledge
and listed as one of the ten main goals of the Croatian nutritional
policy in 1999 [22]. Montenegro’s Ministry of Health in 2009
published „Action plan for nutrition and food safety in Montenegro
2010 – 2014“ [19], and the Republic of Serbia in 2010 published
National program for prevention [4]. As noted by Gurinović et al.
development of the national program in Serbia was necessary because
several studies on quality of nutrition in Serbia together with the
statistical data on mortality and morbidity rates due to CVDs showed
the need for more intensive preventive action [23].
WHO defined dietary goals for the prevention of CVDs that should be
met by all countries. European Heart Network [20] published
nutritional guidelines for the prevention of CVDs on the European
level. Dietary guidelines include regular physical activity (60 to
80 minutes of moderate or 30 minutes of intensive physical activity
per day), decrease in body mass index (BMI) (goal is BMI of 23
kg/m2), while mainly focusing on intake of fat, fresh fruits and
vegetables, dietary fibers and salt [21].
While planning a diet for a patient with CVD or a person at high
risk of CVDs the highest importance has fat intake, and more
importantly sources of that fat [21]. Plant based fats (oils) should
be a main fat source while planning their diet because animal fats
present significant source of saturated fatty acids (FA) [18, 24].
Earlier guidelines were focused on lower intake of cholesterol, but
today the shift has been made towards saturated FA intake [25].
Intake of saturated FA should be restricted to less than 10% of the
total energy derived from fats (overall intake of fats should be
less than 30% of the total energy intake) [21]. Also, intake of
trans-FA should be less than 2% of the total energy intake from fats
[21]. Substitution of saturated FA from animal sources with mono and
polyunsaturated FA from plant sources should lead to reduction of
blood cholesterol level [18, 26]. Official reports show that the
intake of trans-FA is far beyond the recommended with the United
Kingdom and the United States of America having the highest intakes
[6]. Another important aspect is marketing and television
advertising of sweets and fast food, which are the two food groups
that represent the main source of trans FA in daily diet.
Advertising of these products is considered a direct predictor of
trans FA intake [27].
The INTERSALT study correlates the surplus intake of salt to the
higher arterial blood pressure and increased risk of CVDs [28].
Moreover, large number of studies has shown that even slight
decrease in dietary intake of salt leads to decreased arterial blood
pressure [29]. A prospective study conducted in Finland on 2436 men
and women aged 25-64 years showed clear correlation between
increased intake of salt and increased risk of CVDs. This study
shows that salt intake over 6g/day shows 56% increased risk of
coronary disease, 36% increased risk of CVD death, and 22% increased
risk of all cause mortality [30]. Therefore, accomplishing intake of
up to 6g/day of salt is considered as an effective preventive
measure from CVDs [18, 31]. This goal for salt intake is the main
objective of the Croatian initiative CRASH [25, 32], and the
Strategic plan for prevention and control of noncommunicable
diseases in the Republic of Serbia [33]. Despite large number of
national programs targeting lower intake of salt, salt intake
remains elevated around the world. The highest intake of salt was
found in Hungary of 17 g/day/person, with excessive 12 g [6].
Alcohol consumption in high amounts is correlated to increased death
rate, especially due to CVDs [6]. Still, results are inconsistent.
Large number of studies showed relatively small risk of CVDs for
moderate alcohol consumption [18, 34-36]. However, alcohol also
shows some positive effects like increases level of HDL cholesterol
and lowers thrombocyte activity [34, 35], which directly reduces the
risk of thrombosis that lies behind the etiology of CVDs.
Developing a diet plan for a patient with CVD usually includes
consideration of one of the two approaches. The first one is the
Dietary Ap-proaches to Stop Hypertension, or so called the DASH diet
[37]. This approach is based on a low intake of saturated fats and
sodium with increased intake of fruits and vegetables combined with
low fat dairy products [37]. The other approach is the Mediterranean
diet, which was confirmed by the Lyon Diet Heart Study and the
PREDIMED study to have direct correlation to lower mortality rate,
especially due to CVDs [18, 38, 39].
Mediterranean Diet – The Definition
Keys presented the first Mediterranean diet (MD) definition. He
proved, for the first time, health benefits of the MD in a research
encompassing more than 12 700 people from seven Mediterranean
countries [40]. In Croatia, several studies dealing with the dietary
habits of inhabitants on isolated island have been conducted [41].
All showed that even though the diet of islanders is (eg. Vis, Mljet)
fundamentally Mediterranean, there is a shift that can be noticed.
This shift is seen in increased consumption of industrial products,
sugar and read meat, which coincides with lower consumption of fish,
fruits and vegetables
[41]. Although in their diets there is some traditional MD present
many islanders show unfavourable shift in their dietary patterns
[42]. These findings are in accordance with the increased problems
related to CVDs among researched islanders [41].
Even though there is no such thing as one MD, some characteristics
are shared. These are: a) high intake of fats (more than 40% of
total energy intake), mostly from olive oil; b) high intake of
wholegrain, fruits, vegetables, legumes and nuts; c) moderate to
high consumption of fish; d) moderate to low consumption of white
meat (poultry or rabbit meat) and dairy products, mostly yoghurt or
fresh cheese; e) low consumption of red meat and meat products; f)
moderate consumption of red wine with meal [43, 44]. The last MD
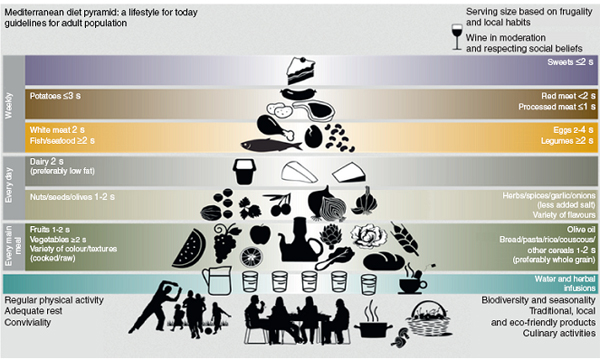
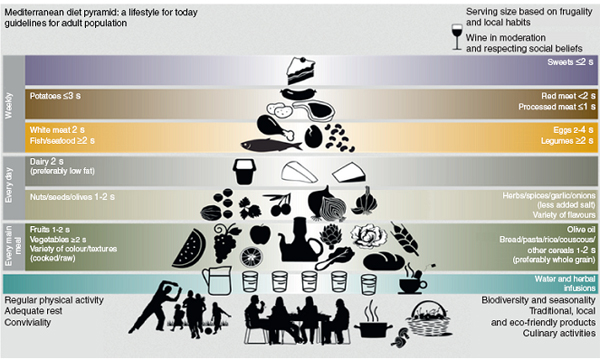
pyramid (Picture 2) includes two main changes related to consumption
of cereals and dairy products. By and large, these relate to intake
of wholegrain and low fat dairy products. In addition, physical
activity, socialization and psychosocial aspects related to dining
with friends and family have been added to the pyramid [43].
Picture 2 The Mediterranean diet pyramid [43]
Mediterranean Diet’s Characteristics
Discussions on the MD usually imply that the MD is a diet rich in
fats. However, there are different types of the MD. Some are high in
fats (Greece) and other are quite low in fats (South Italy, South
France) [40, 45]. For example, the Lyon study researched a low fat
content [10, 40] with the main fat source being canola oil margarine
not olive oil [45].
Beneficial effect on cardiovascular health olive oil owns to its FA
profile. Mono and polyunsaturated FA reduce blood cholesterol level
and risk of heart diseases when they substitute one portion of
saturated FA in the diet. The most common FA from the family of
monounsaturated FA is oleic acid, the main FA of olive oil [47]. Due
to its high content in olive oil and other antioxidants, consumption
of olive oil reduces LDL cholesterol simultaneously affecting HDL
cholesterol. Additionally, this composition of olive oil prevents
oxidation of LDL cholesterol [47, 48]. Also, olive oil contains
other components out of which plant sterols, and beta-sitosterols
are the most important in reduction of cholesterol levels [25, 47].
Therefore, olive oil has several protective mechanisms on
atherosclerosis.
Fish is a food group with almost ideal nutritional profile. They are
rich in essential FA, ome-ga-3 FA and proteins [24, 43]. Two main
omega-3 FA in fish are eicosapentaenic (EPA) and docohex-aenoic
acids (DHA). It has been proved that supplementation of 2 to 4 g of
omega-3 FA/day in patients with increased triglycerides will reduce
their triglycerides by 25 to 30%. Additionally, 1 g/day of omega-3
FA given to patients after recovered myocardial infarction
significantly reduces overall mortality and risk of sudden death due
to arrhythmia [46].
Studies have shown that the MD long-term leads to weight loss,
change in BMI, systolic and diastolic blood pressure, fasting blood
glucose level, total cholesterol and endothelial inflammation
indicator and high-sensitivity C-reactive protein (hs-CRP) [45, 49].
The largest hospital in Croatia, University Hospital Centre Zagreb
provides its patients with hypolipemic MD since 2011 [50].
One of the main additional characteristics of the MD is moderate
consumption of red wine [43]. Phenols from red wine, especially
resveratrol (also present in red grapes), decrease oxidation of LDL
cholesterol, causatively affecting atherogenicity, act as an
anti-aggregation, and antiinflammatory agents, and diminish
thrombocyte aggregation, contributing to possible anti
atherosclerotic effects. Significant part of wine’s protective
effects can be attributed to HDL cholesterol increase [25, 35, 51].
Mediterranean Diet and Health Benefits
After publication of the results of the Lyon Diet Heart Study
(Lyon) [40], number of studies reported on various health benefits
of the MD. In 2003 Trichopoulou et al. published the first modern
epidemiological study that examined impact of the MD on different
health aspect [52]. This prospective follow-up study encompassed 22
043 adult Greeks, and was observing their diet with so called
Mediterranean score. Study found that the higher the score was, the
lower mortality rate from CVDs was. Final data showed that mortality
rate from CVDs and cancers was inversely correlated to higher MD
compliance [52], and the study confirmed earlier findings from the
Lyon study [10, 40]. Higher compliance to the MD correlates to the
lower prevalence of obesity [53], which was also confirmed by
Croatian studies [41, 42]. Meta-analysis published in 2010 summed-up
the whole inverse relation between the MD, CVDs and overall
mortality [39]. Additionally, meta-analysis pub-lished in 2011
showed that the MD has higher protective effect on health than a low
fat diet [49].
The last large prospective study conducted in Spain, the PREDIMED
study, have shown that adoption of the MD leads to 30% reduction in
complications due to hearth diseases, and 40% lower risk of heart
attack, which was based on a 5 year follow-up [54]. In addition,
this study confirmed earlier findings; the importance in primary
prevention from the Lyon study [10, 40], epidemiologic significance
from the aspects of morbidity and mortality [39, 52] from CVDs, as
well as from cancers, dementia, and the risk of Alzheimer’s disease
[55-57]. Furthermore, Skarupski et al. [58] showed that dietary
pattern that is more in accordance to the MD (based on MedDietScore
principle) shows potential in reducing depression among people of 65
years and older.
Recently, more emphasis is put on possibilities to modify the MD for
non-Mediterranean populations, seeing it as a possible solution for
noncommunicable diseases [59]. This is due to a large number of
prospective studies performed in the non-Mediterranean countries
that, besides already determined effect of the MD, show MD’s
potential to protect from premature death [60-64], and
cerebrovascular diseases [65].
CONCLUSION
For years, Mediterranean diet is on the top of scientific
interest. The reason lies in proven correlation with CVDs
prevention, and causatively lower mortality and morbidity due to
CVDs. Moreover, this effect was found for other noncommunicable
chronic diseases, from cancers to dementia. The Mediterranean diet
is not just a specific dietary regime; it represents a way of life.
Characteristic combinations of foods, with some specifics between
Mediterranean countries make it plain and complicated at the same
time. Undoubtedly, the Mediterranean diet will keep on positioning
itself as one of the possible solutions to global issues related to
CVDs.
LITERATURE
- World Health Organization. Cardiovascular diseases, Fact
sheet No 317. World Health Organization, 2013. Available from:
http://www.who.int/cardiovascular_diseases/en
- Hrvatski zavod za javno zdravstvo. Umrle osobe u Hrvatskoj u
2011. godini. Hrvatski zavod za javno zdravstvo, Služba za javno
zdravstvo, Zagreb, 2012.
- Ministarstvo zdravlaj Crne Gore. Akcioni plan za ishranu i
bezbjednost hrane Crne Gore 2010-2014. Ministarstvo zdravlja
Crne Gore, Podgorica, 2009.
- Službeni glasnik Republike Srbije. Uredba o nacionalnom
programu prevencije, lečenja i kontrole kardiovaskularnih
bolesti do 2020. godine. Službeni glasnik Republike Srbije br.
11/2010, Beograd, 2010.
- Institut za javno zdravlje Srbije „Dr. Milan Jovanović
Batut“. Zdravlje stanovnika Srbije – analitička studija 1997-
2007. Institut za javno zdravlje Srbije, Beograd, 2008.
- World Health Organization. Global Atlas on cardiovascular
disease prevention and control. Geneva: World Health
Organization; 2011.
- American Heart Association (AHA). Understand your risk of
heart attack. 2012. Available from:
www.heart.org/HEARTORG/Conditions/HeartAttack/
UnderstandYourRiskofHeartAttack/Understand-Your-Risk-of-Heart-Attack_UCM_002040_Article.jsp
- Singh M, Lennon RJ, Holmes DR Jr, Bell MR, Rihal CS.
Correlates of procedural complications and a simple integer risk
score for percutaneous coronary intervention. J Am Coll Cardiol
2002; 40(3): 387-93.
- International Diabetes Federation. IDF Diabetes Atlas, 6th
edition. IDF; 2013.
- De Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye
J, Mamelle N. Mediterrranean Diet, Traditional Risk Factors, and
the Rate of Cardiovascular Complications After Myocardial
Infarction: Final Report of the Lyon Diet Study. Circulation
1999; 99(6): 779-85.
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM,
Strath SJ et al. Compendium of physical activities: An update of
activity codes and MET intensities. Med Sci Sports Exerc 2000;
32(9 suppl): S498-504.
- Warburton DER, Nicol CW, Bredin SSD. Health benefits of
physical activity: the evidence. CMAJ 2006; 174(6): 801-9.
- World Health Organization. A global brief on hypertension.
Geneva: World Health Organization; 2013.
- World Health Organization. WHO Update on smoking. Fact sheet
No 339. World Health Organization, 2013. Available from:
http://www.who.int/mediacentre/factsheets/fs339/en/
- Demarin V, Lisak M, Morović S. Mediterranean Diet in Healthy
Lifestyle and Prevention of Stroke. Acta Clin Croat 2011; 50(1):
67-77.
- Bédard A, Riverin M, Dodin S, Corneau L, Lemieux S. Sex
differences in the impact of the Mediterranean diet on
cardiovascular risk profile. Brit J Nutr 2012; 108: 1428-34.
- Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL,
Jameson JL et al. Harrison's Principles of Internal Medicine,
17th edition. New York: Mc-Graw Hill Medical; 2008.
- Verschuren WMM. Diet and Cardiovascular Disease. Curr
Cardiol Rep 2012; 14: 701-8.
- Cholesterol Treatment Trialists' Collaborators. Efficacy and
safety of cholesterol-lowering treatment: prospective
meta-analysis of data from 90 056 participants in 14 randomised
trials of statins. Lancet 2005; 366: 1267-78.
- Haveman-Nies A, de Groot LP, Burema J, Cruz JA, Osler M, van
Staveren WA. Dietary quality and lifestyle factors in relation
to 10-year mortality in older Europeans: the SENECA study. Am J
Epidemiol 2002; 156: 962-8.
- Bhupathiraju SN, Tucker KL. Coronary heart disease
prevention: Nutrients, foods, and dietary patterns. Clinica
Chimica Acta 2011; 412(17-18): 1493-514.
- Ministarstvo zdravstva i Hrvatski zavod za javno
zdravstvo.Hrvatska prehrambena politika. Hrvatski zavod za javno
zdravstvo, Zagreb, 1999.
- Gurinović M, Ristić-Medić D, Vučić V, Milešević J,
Konić-Ristić A, Glibetić M. Ishrana i kardiovaskularne bolesti.
Acta Clinica 2013;13(1):156-68.
- Vrca Botica M, Pavlić Renar I i sur. Šećerna bolest u
odraslih. Zagreb: Školska knjiga; 2012.
- Reiner Ž. Uloga prehrane u prevenciji i terapiji
kardiovaskularnih bolesnika. Medicus 2008; 17: 93-103.
- Vaccarino V. The Mediterranean Diet in Cardiovascular
Disease. U Trovato GM urednik. The Mediterranean Diet: A
resources for Medicine, An opportunity for Italy. Italija:
Dietamed, 2010.
- Raine KD, Lobstein T, Landon J, Potvin Kent M, Pellerin S,
Caulfield T et al. Restricting marketing to children: Consensus
on policy interventions to address obesity. Journal of Public
Health Policy 2013; 34(2): 239-53.
- Stamler J. The INTERSALT study: background, methods,
findings, and implications. Am J Clin Nutr 1997; 65(suppl):
626S-42S.
- Dumler F. Dietary sodium intake and arterial blood pressure.
J Ren Nutr 2009;19:57-60.
- Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V,
Tanskanen A, Pietinen P et al. Urinary sodium excretion and
cardiovascular mortality in Finland: a prospective study. Lancet
2001; 357: 848-51.
- Asaria P, Chisholm D, Ezzati M, Beaglehole R. Chronic
disease prevention:Health effects and financial costs of
strategies to reduct salt intake and control tobacco use. Lancet
2007; 370: 2044-53.
- Jelaković B, Kaić-Rak A, Miličić D, Premužić V, Skupnjak B,
Reiner Ž. Manje soli – više zdravlja. Hrvatska inicijativa za
smanjenje prekomjernog unosa kuhinjske soli (CRASH). Liječnički
vijesnik 2009; 131: 87-92.
- Ministarstvo zdravlja Republike Srbije. Strategija za
prevenciju i kontrolu hroničnih nezaraznih bolesti Republike
Srbije. Awailable from:
http://www.minzdravlja.info/downloads/Zakoni/Strategije/Strategi-ja
Za Prevenciju I Kontrolu Hronicnih Nezaraznih Bolesti.pdf
- Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de
Gaetano G. Alcohol Consumption and Mortality in Patients With
Cardiovascular Disease: A Meta-Analysis. J AM College Cardiol
2010; 55(13): 1339-47.
- Klatsky AL. Alcohol and cardiovascular health. Physiology &
Behavior 2010; 100(1): 76-81.
- Beulens JWJA, Soedamah-Muthu SS, Visseren FLJ, Grobbee DE,
van der Graaf Y. Alcohol consumption and risk of recurrent
cardiovascular events and mortality in patients with clinically
manifest vascular disease and diabetes mellitus: The Second
Manifestations of ARTerial (SMART) disease study.
Atherosclerosis 2010; 12(1): 281-6.
- Appel LJ, Thomas MPH, Moore J, Obarzanek E, Vollmer WM,
Svetkey LP et al. A clinical trial of the effect of dietary
patterns and blood pressure management. N Eng J Med 1997; 336:
1117-24.
- Tracy SW. Something new under the sun? The Mediterranean
diet and cardiovascular health. N Engl J Med 2013; 368(14):
1274-6.
- Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on
benefits of adherence to theMediterranean diet on health: an
updated systematic review and meta-analysis. Am J Clin Nutr
2010; 92(5): 1189-96.
- De Lorgeril M. Mediterranean Diet and Cardiovascular
Disease: Historical Perspective and Latest Evidence. Curr
Atheroscler Rep 2013; 15: 370.
- Missoni S. Nutritional Habits of Croatian Island Populations
– Recent Insights. Coll. Antropol 2012; 36(4): 1139-1142.
- Sahay RD, Couch SC, Missoni S, Sujoldžić A, Novokmet N,
Duraković Z et al. Dietary Patterns in Adults from an Adriatic
Island of Croatia and Their Associations with Metabolic Syndrome
and Its Components. Coll Antropol 2013; 37(2): 335-42.
- Aros F, Estruch R. Mediterranean Diet and Cardiovascular
Prevention. Rev Esp Cardiol 2013;66(10):771-4.
- Schroder H. Protective mechanism of the Mediterranean diet
in obesity and type 2 diabetes. J Nutr Biochem 2007; 18(3):
149-60.
- Di Daniele N, Petramala L, Di Renzo L, Sarlo F, Della Rocca
DG, Rizzo M et al. Body composition changes and cardiometabolic
benefits of a balanced Italian Mediterranean Diet in obese
patients with metabolic syndrome. Acta Diabetol 2013; 50:
409-16.
- Delgado-Lista J, Perez-Caballero AI, Perez-Martinez P,
Garcia-Rios A, Lopez-Miranda J, Perez-Jimenez F. Mediterranean
Diet and Cardiovascular Risk. U: Gasparyan AY urednik.
Cardiovascular Risk Factors. InTech, 2012.
- Farràs M, Valls RM, Fernández-Castillejo S, Giralt M, Solà
R, Subirana I et al. Olive oil polyphenols enhance the
expression of cholesterol efflux related genes in vivo in
humans. A randomized controlled trial. J Nutr Biochem 2013;
24(7): 1334-9.
- Widmer RJ, Freund MA, Flammer AJ, Sexton J, Lennon R, Romani
A et al. Beneficial effects of polyphenolrich olive oil in
patients with early atherosclerosis. Eur J Nutr 2013; 52:
1223-31.
- Nordmann AJ, Suter-Zimmermann K, Bucher HC, Shai I, Tuttle
KR, Estruch R et al. Meta-Analysis Comparing Mediterranean to
Low-Fat Diets for Modification of Cardiovascular Risk Factors.
Am J Med 2011; 124: 841-51.
- Krznarić ž, Vranešić Bender D, Pavić E. Prehrana bolesnika s
metaboličkim sindromom. MEDIX 2011; 17(97): 156-9.
- Quiñones M, Miguel M, Aleixandre A. Beneficial effects of
polyphenols on cardiovascular disease. Pharmacological Research
2013; 68(1): 125-31.
- Trichopoulou A, Costacou T, Bamia C, Trichopoulos D.
Adherence to a Mediterranean Diet and Survival in a Greek
population. N Engl J Med 2003; 348: 2599-608.
- Bonaccio M, Di Castelnuovo A, Costanzo S, De Lucia F,
Olivieri M, Donati MB et al. Nutrition knowledge is associated
with higher adherence to Mediterranean diet and lower prevalence
of obesity. Results from the Moli-sani study. Appetite 2013; 68:
139-46.
- Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D,
Arós F et al. Primary prevention of cardiovascular disease with
a Mediterranean diet. N Engl J Med 2013; 368(14): 1279-1190.
- Shah, R. The role of nutrition and diet in Alzheimer
disease: a systematic review. J Am Med Dir Assoc 2013; 14(6):
398-402.
- Lourida I, Soni M, Thompson-Coon J, Purandare N, Lang IA,
Ukoumunne OC et al. Mediterranean diet, cognitive function, and
dementia: a systematic review. Epidemiology 2013; 24(4): 479-89.
- Sofi F, Macchi C, Casini A. Mediterranean Diet and
Minimizing Neurodegeneration. Curr Nutr Rep 2013;2:75-80.
- Skarupski KA, Tangley CC, Li H, Evans DA, Morris MC.
Mediterranean diet and depressive symptoms among older adults
over time. The Journal of Nutrition, Health & Aging 2013; 17(5):
441-5.
- Hoffman R, Gerber M. Evaluating and adapting the
Mediterranean diet for non-Mediterranean populations: A critical
appraisal. Nutr Rev 2013; 71(9): 573-84.
- Hoevenaar-Blom MP, Nooyens AC, Kromhout D, Spijkerman AM,
Beulens JW, van der Schouw et al. Mediterranean style diet and
12-year incidence of cardiovascular diseases: the EPICNL cohort
study. PLoS One 2012; 7(9): e45458.
- Martínez-González MA, Guillén-Grima F, De Irala J,
Ruíz-Canela M, Bes-Rastrollo M, Beunza JJ et al. The
Mediterranean diet is associated with a reduction in premature
mortality among middle-aged adults. J Nutr 2012; 142(9) :1672-8.
- Gardener H, Wright CB, Gu Y, Demmer RT, Boden-Albala B,
Elkind MS et al. Mediterranean-style diet and risk of ischemic
stroke, myocardial infarction, and vascular death: the Northern
Manhattan Study. Am J Clin Nutr 2011; 94(6): 1458-64.
- Tognon G, Lissner L, Sæbye D, Walker KZ, Heitmann BL. The
Mediterranean diet in relation to mortality and CVD: a Danish
cohort study. Br J Nutr 2013; 3: 1-9.
- Hodge AM, English DR, Itsiopoulos C, O'Dea K, Giles GG. Does
a Mediterranean diet reduce the mortality risk associated with
diabetes: evidence from the Melbourne Collaborative Cohort
Study. Nutr Metab Cardiovasc Dis 2011; 21(9): 733-9.
- Misirli G, Benetou V, Lagiou P, Bamia C, Trichopoulos D,
Trichopoulou A. Relation of the traditional Mediterranean diet
to cerebrovascular disease in a Mediterranean population. Am J
Epidemiol 2012; 176(12): 1185-92.
|
|
|
|