| |
|
|
INTRODUCTION
Patients with malignant diseases need multidisciplinary approach
and therapy that is often given intravenously. Central vein
catheters (CVC) have very important role in the cure of these
patients. They are used not only in the application of chemotherapy
but also for the extended usage of liquids, blood and blood
derivatives, antibiotics, total parental nutrition as well as for
common blood analysis. There are different types of CVC: non -tunneled
CVC, peripheral inserted PICC, tunneled and CVC with implantable
port. For oncological patients the most adequate is CVC with
implantable port due to relatively simple implantation and uses, low
infection levels, safety and comfort that provides to patients
[1,2,3,4]. In modern oncology these systems replace the tunneled
catheters and short – term use. Chemotherapy is taken cyclically and
to avoid reuse of CVC that leads to sclerosis of the blood vessel
wall and as every invasive procedure takes its risks (infection,
hematoma, pneumothorax…), there is a possibility of implementation
port – a – chat catheter that improves lives to patients on long
termed therapies [5].
PROCEDURE DESCRIPTION: PORT-A-CATH PLACEMENT
Port-a-cath is composed of the catheter and the chamber that is
apart from the cytostatic treatment, antibiotics and painkillers
also used for parental nutrition or for the blood sampling. The port
is placed subcutaneously, mostly on the front of the chest,
connected with the catheter positioned in superior vena cava above
the confluence in right atrium.
Port-a-cath can stay placed for several months. To enable the route
for therapy taking or blood sampling the special hollow needle
(Huber needle) is implemented through the skin in silicon membrane
of the port whilst the chamber is immobilized with fingers of non
dominant hand. The port puncture is always done in sterile
conditions with application of aseptic technique on the skin with
usage of sterile gloves to prevent infection [1]. It is recommended
to rinse the port after each usage with heparin solution in
concentration of 10-100ij/ml . [6]
The procedure of port-a-cath catheter placement can be done in
following ways: by surgery technique of the preparation of blood
vessel , by the technique of direct vein puncture lead by
ultrasound. The advantage of direct vein puncture is the possibility
of performing the procedure in local anesthesia. Surgery placement
of the port is to be done in the general or regional anesthesia. The
potential places for insertion of CVC are cephalic and basilic vein,
subclavian vein, vein jugular intern on the neck or vein jugular
extern that can be used as the approach at children. The choice of
the place of vein puncture is usually determined on the basis of
localization of the malignant disease (contralateral side at
unilateral breast cancer), the presence of infection, vein
thrombosis or previously placed pace – maker . The average length of
the catheter to reach the wanted position (till cavoatrialjunction)
when punctured jugular or vein subclavian is 18 cm on the right side
and 22 cm on the left side. During the procedure EKG monitoring is
necessary. After the procedure the position of the catheter is
checked by the lung x-ray which excludes the presence of
pneumothorax as well. [2]
The most common complication though and the most common reason of
catheter explantation is infection and that is why the antimicrobial
prophylaxis is necessary. [7]
Other complications can be divided according to time of origin as
follows:
- complications during the intervention (puncture of artery,
hematoma, air embolism, pneumothorax , heart arrhythmias,
perforation of heart hollows and big blood vessels)
-complications related to catheter (dislocation, thrombosis,
occlusion, rupture of catheter, narcosis of skin)
-vascular complications (thrombosis of vein vessel, arterial vein
malformations )
Other division of complications related to the implantation of
port-a-cath system is as follows:
-early (between 24 hours and 4 weeks from implantation)
-late (4 weeks after implatation ) [3]
The purpose of the work was to present the experience of Clinical
Hospital Center Bezanijskakosa related to implantation of port-a-cath
catheter.
Method
Implantation of port-a-cath system presents the procedure that is
performed in operation room under local anesthesia in aseptic
conditions.
All the patients needed frequent parental therapy taking and blood
sampling for lab analysis and the indication for implantation of S
port-a-cath system was set up by an oncologist or a surgeon.
Due to compromised immunology status and prevention of the catheter
infection all the patients got the prophylactic dose of antibiotics
Ceftriacson 2 g an hour before the procedure.
The placement mostly was set up in the right veinsubclavian whilst
with the female patients that were exposed to total mastectomy port
was placed on the opposite side. In the conditions of local
anesthesia catheter was placed by the technique of direct puncture
of vein on the basis of anatomy points. In front of pectoral muscle
the pocket in subcutaneous tissue was made where the chamber was
positioned and fixed. In the end of the procedure the chamber was
rinsed with the solution of heparin in concentration of 100ij/ml.
After the procedure the position of catheter was verified by the x-
ray.
The patients and the accompanied families were educated for the
usage, rinse and infection prevention of the port-a-cath system.
RESULTS
In our institution since January 2017 until 31st January 2018.,
16 port-a-cath vascular catheters were implanted to oncologic
patients.
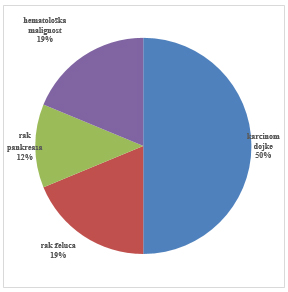
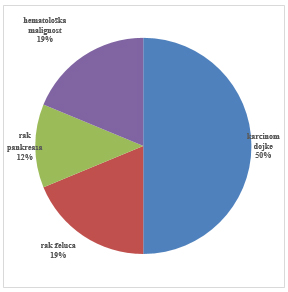
The highest percentage of the patients got the therapy for the
breast cancer [8], 3 patients were treated from the stomach cancer,
2 from pancreas cancer and bile ducts and 3 patients had
hematological malignity (Figure 1). The patients in average were
aged 48 (27 – 75).
Figure 1: Distribution of oncologic patients
underwent the port-a-cath implantation
There were no early complications during the placing of the port.
Two patients had late complications - dislocation of the catheter
with one that led to renewed insertion of port and the other patient
had the rotation of port chamber that was solved in the local
anesthesia.
DISCUSSION
In developed countries the usage of these catheters is standard
in the treatment of oncologic patients whilst in developing
countries the data about the usage of these catheters is poor,
probably due to inaccessibility and the high costs of the catheters.
Port-a-cath systems are closed and their purpose is to provide
access to the central vascular system. It gives possibility to use
the skin as a natural barrier against infection and to take out a
puncture needle after each usage. The advantages of such a close
system are decreased possibility of infection, simple maintenance of
the port that is not in use, esthetic benefit of subcutaneously
positioned chamber, providing the mobility of patients as well as
doing their normal daily activities and decreased possibility of
complications related to central and peripheral venous catheters.
[1]
Infections, hematoma, malposition of the catheter, pneumothorax,
thrombosis, embolization, catheter knicking are still important
complications that follow the implementation of a port – a – chat
catheter. During the last decade the reports indicate that the rate
of complications has been reduced significantly due to improvement
of the placing technique it self as well as the material of the
catheter. Previously Hicman and Borivac catheters were used and
nowadays port - a - chat catheters are used due to easy
accessibility and lower rate of complications. [8,9]. As the
technology of producing catheters and materials has been improved,
nowadays catheters with implantable port are lighter, stronger and
can support higher pressure of the liquids for frequent diagnostic
procedures that the malignant patients are exposed to. [10-17]
In our experience, this procedure was accompanied with late
complications occurred in 12.5% of patients. Dislocation of the
catheter that led to renewed insertion of port occurred in 6.25% and
also, in 6.25% of patients the rotation of port chamber occurred.
These complications were resolved routinely and did not
significantlly affect the treatment protocol.
Advantages of this procedure were numerous. Reuse of standard CVC
sometimes leads to sclerosis of the blood vessel. The veins of the
patients with port-a-cath systems were protected and the
reimplantation of CVC is avoided, except for one patient due to
dislocation of the catherter. Also, using port-a-cath systems had
benefits for medical care and other treatment procedures providing a
greater comfort to medical staff by simple approach to vein route.
Subjective assessment of all the patients with implanted port-a
-chat system is improved quality of life. The main advantages
observed by patients were greater mobility and improved comfort.
CONCLUSION
Placing of port-a-cath system significantly improves the quality
of life in the following ways:
The veins of the patients were protected from sclerosis
reimplantation of CVC is avoided. Medical staff has simple approach
to the vein route for therapy giving or blood sampling for the lab
analysis. Patients experienced greater mobility and comfort.
LITERATURE:
- Gonda SJ, Li R. Principles of subcutaneous port placement.
Tech Vasc Interv Radiol. 2011;14(4):198-203.
- Teichgräber UK, Pfitzmann R, Hofmann HA. Central venous port
systems as an integral part of chemotherapy. Dtsch Arztebl Int.
2011;108(9):147-53.
- Teichgräber UK, Gebauer B, Benter T, Wagner HJ Central
venous access catheters: radiological management of
complications. Cardiovasc Intervent Radiol. 2003; 26(4):321-33.
- Torro A. Shembari E, Mattone E. Di Carlo I Which is better
for patients with breast cancer : Totally implanted vascular
access device or peripheral inseted central catheter (PICC)?
World J Surg. 2020;44(3):1004-1005. doi:
10.1007/s00268-019-05196-4
- Di Carlo I, Pulvirenti E, Mannino M, Toro A. Increased use
of percutaneous technique for totally implantable venous access
devices. Is it real progress? A 27-year comprehensive review on
early complications. Ann Surg Oncol 2010;17:1649–1656.
- Teichgräber UK, Gebauer B, Benter T, Wagner Jrofo. Long-term
central venous lines and their complications.
2004;176(7):944-52.
- Gebauer B, Teichgräber U, Werk M, Wagner HJ Rofo.
Periinterventional prophylactic antibiotics in radiological port
catheter implantation. 2007;179(8):804-10.
- Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK,
Weinstein RA. Effectiveness of chlorhexidine bathing to reduce
catheter-associated bloodstream infections in medical intensive
care unit patients. Archives of Internal Medicine
2007;167(19):2073-9. [PUBMED: 17954801]
- Boonyasiri A, Thaisiam P, Permpikul C, Judaeng T, Suiwongsa
B, Apiradeewajeset N, et al. Effectiveness of chlorhexidine
wipes for the prevention of multidrug-resistant bacterial
colonization and hospital-acquired infections in intensive care
unit patients: a randomized trial in Thailand. Infection Control
and Hospital Epidemiology 2016;37(3):245-53. [PUBMED: 26894621]
- Walser EM. Venous access ports: indications, implantation
technique, follow-up, and complications. Cardiovasc Intervent
Radiol. 2012;35(4):751-64.
- Xing, Lei, Wu Kainan. Diagnosis and treatment of
peripherally inserted central catheters (PICC)-related sepsis in
breast cancer for chemotherapy. The Chinese-German Journal of
Clinical Oncology. Pub Date : 2012-02-08. DOI:
10.1007/s10330-011-0912-6.
- Lewis SR, Schofield-Robinson OJ, Rhodes S, Smith AF.
Chlorhexidine beating of the critically ill for the prevention
of hospital-acquired infection. Cochrane Database Syst Rev.
2019;8(8):CD012248. doi: 10.1002/14651858.CD012248.pub2.
- OkszakiM,Oyama K, Kinoshita J , at al. Incidence of and risk
factors for totally implantable vascular access device
complications in patients with gastric cancer: A retrospective
analysis. Mol Clin Oncol. 2019;11(4):343-348. doi:
10.3892/mco.2019.1897. Epub 2019 Jul 15.
- Goltz JP, Noack C, Petritsch B, Kirchner J, Hahn D, Kickuth
R. Totally implantable venous power ports of the forearm and the
chest: Initial clinical experience with port devices approved
for high-pressure injections. Br J Radiol. 2012;85:e966–e972.
doi: 10.1259/bjr/ 33224341.
- Schiffer CA, Mangu PB, Wade JC, Camp-Sorrell D, Cope DG, El-Rayes
BF, Gorman M, Ligibel J, Mansfield P, Levine M. Central venous
catheter care for the patient with cancer: American Society of
Clinical Oncology clinical practice guideline. J ClinOncol.
2013;31:1357–1370. doi: 10.1200/JCO.2012.45.5733
- Li Y, Cai Y, Gan X, Ye X, Ling J et al. Application and
comparison of different implanted ports in malignant tumor
patients. World J Surg Oncol. 2016;14:251. doi:
10.1186/s12957-016-1002-6.
- Ji L, Yang J, Miao J, Shao Q, Cao Y, Li H. Infections
related to totally implantable venous-access ports: Long-term
experience in one center. Cell Biochem Biophys. 2015;72:235–240.
doi: 10.1007/s12013-014-0443-1
|
|
|
|