| |
|
|
INTRODUCTION
Although implantology as а science has flourished in recent
decades, it should be remembered that the history of implantology
stretches back to ancient times. Based on archaeological research,
we find that 4,000 years ago, the Chinese used spikes of bamboo
trees and implanted them in the jaw bone as a substitute for lost
teeth. The ancient Egyptians, the Etruscans, and later the
Phoenicians used noble metals, processed ox bones or ivory and
implanted them in bone tissue. These innovative nations used gold
wires to stabilize disassed teeth [1,2].
Hippocrates (5th century BC) wrote about the possibility of
hardening artificial teeth using gold or silk thread to replicate
the teeth removed, advising the practitioner not to "discard the
teeth or teeth removed from the injured mandibula, but to return
them to place, tying them to the remaining teeth with golden threads
"[3]. The same recommendation was made by Aulus Cornelius Celsus
(1st century BC) which in the journal “De Medicina” mentioned the
possibility of replacing the missing tooth with a dental implant,
taken from the kadaver, in those who lost a tooth for different
reasons; however, he did not report whether such treatment was
successful. However , it must be noted that the main purpose of
these replacements was cosmetic , while the function of mastication
was not much considered [3].
It is known that Mayans in the 7th century used various materials
for aesthetic purposes, such as tirkes, quartz, serpentine, etc. and
inserted carefully prepared spaces on the vestibular surfaces of
mostly front teeth. Particularly interesting is the findings of
Wilson Popenoe and his wife Dorothy during a survey of the Mayan
civilization in Honduras, where they found a fragment of mandibula
containing three replica teeth made of shellfish in alveolas. In
studying this unusual find, expedition members initially assumed
that the inserted elements were cosmetic treatments post-mortem,
possibly as part of a complicated funeral ritual or religious
practice [4].
Picture 1. The find of a 7th-century mandle of the
Mayan civilization was found in Honduras. (Taken from
http://www.implantmn.com/about-dental-implants/history-and-types-of-dental-implants/
for scientific purposes and not used for commercial purposes)

Radiographs of mandible in 1970. showed the formation of a bone
around the implants that resembles what is seen around modern
implants. This appears to have been the first authentic aloplastic
material implanted in human tissue during life. Recent and
exhaustive histological research on the behaviour of shell fragments
in direct contact with bone tissue in experiments with animals has
confirmed the principle of oseointegration between the two tissues
[3,6,7].
Until the mid-19th century numerous attempts at replantation and
dental transplantation were recorded, where the works of Pare,
Dupont, Fauchard and others were not much advanced in the
development of implantology. In the 19th and early 20th centuries,
the founders of the Baltimore School, further Maggiolo, Bonville,
Gram, Paine and others used various materials, platinum, lead,
silver, gold, iridium, ceramics, and used cylinder-shaped implants,
hollow screws, full screws, cylindrical nets, spirals, needles, etc.
Although these cases cannot be considered entirely successful, it
must be noted that during this century, from Maggiolo to Paine,
researchers have progressively tried, at least on a conceptual
level, to use more and more inert materials, and this is in
accordance with the development of the concept of implanting
aloplastic implants with retentional morphology [6,7].
In 1938, Sweden's Gustav Dahl installed a subperiostal mandibular
implant with four metal columns above the gums that were later
anchored to the braces.It is important to note that after this
attempt, the Swedish Dental Society asked him to immediately refrain
from conducting the treatment, and the punishment was expelled from
society at the very moment when the procedure appeared destined for
success [8,9].
In Boston in 1939. the Strock brothers began testing of vitalium
implants, chromium alloys, molibden and cobalt that they had already
tested on dogs. The design of subperiosteal implants was further
explored and developed by Lew, Baush and Berman in 1950. [8,9]. At a
conference in Milan on 27 february 1947. Italy's Manlio Formiggini
proposed a hollow spiral bolt made of stainless steel wire or tantal.
The Designer called the method "direct endoalveolar implantation"
and marked a definitive transition to an era of endoseal implants.
Formigjni then presented several clinical cases and brought with him
two patients who chewed without problems with fixed dentures [9].
The dental world has experienced a justifiable period of cautious
skepticism towards endoseal implants and hopes instead to make the
latest subperiosteal implant technique possible. As a result,
failures (due to technical errors by formigni's first students) were
taken into account more than success when it came to official
verdicts [3, 8,9].
OSSEOINTEGRATION
Osseointegration as a concept is introduced by Per-Ingvar
Branemark (1969), professor at the Institute of Applied
Biotechnology, University of Gothenburg. He defined it as "a direct
structural and functional connection between the living bone and the
surface of the implant". He came to this phenomenon by accident. He
observed microcirculation of the bone and the healing of the wounds
through the titanium tube that he incorporated into the rabbit
fibula. When he tried to remove the chamber after the experiment, he
noticed that it had grown with bone tissue and could not be easily
removed. That's when he discovered bone growth on the surface of the
titanium chamber and good integration of bone implants. The
phenomenon was called oseointegration [11,12,13,14]. Oseointegration
is derived from the Greek word for bone "osteon", and Latin "integrare",
which means to create a whole [11]. It was assumed that bone
anchoring on the principle of feeling could work in humans, and the
first toothless patients were treated in 1965 [11,12,13,14].
At the time, the оsseointegration was not an accepted phenomenon.
Although experiments on animals conducted in Branemark's laboratory
made it clear that it was possible to anchor the bone on the
condition that basic guidelines were observed, the scientific
community was not convinced of the osseointegration because
hystоlogical evidence was absent. It wasn't until mid-1970, A.
Schroeder, using a newly developed technique of cutting non-decalized
bones and implants without separating anchored parts, showed that it
was osseointegration. It was the first evidence of a direct
conection of implants and bone. The original Branemark implant was
created as a cylindrical; later, the conical shapes appeared
[13,14,15]. Implant designs were breakthrought in the 1960s, and the
basic spiral design was modified by Dr Leonard Linkow in 1963. the
implant of the shape of the blade with the ability to place in
maxillo and mandibul, which is now known as endooseal implantation
[8,14].
In 1978, The Harvard Consensus Conference was held to establish a
consensus on the use of implants at Harvard University, and the
standard for a successful implant was whether the implant remained
implanted and functional for five years. This standard may seem
extremely short, but it illustrates what the expectations of implant
treatment were at the time [8,16].
During the 1980s, Professor Zarb of the University of Toronto played
a central role in holding the Toronto Conference on Oseointegration
in Clinical Dentistry, where Branemark presented the results of his
research over 30 years and clinical practice for nearly 20 years.
With this conference as a turning point, the Branemark regime has
expanded across North America. The typical Branemark regime during
this period consisted of implanting four to six implants in the
lower jaw and recommended a surgical two-stage technique that became
widespread worldwide [8,16].
In the mid-1980s, a common implant used by many dentists was a
root-shaped implant. The main factors that determined which implant
system was selected relative to the other, included design, surface
roughness, prosthetic considerations, simplicity of insertion into
the bone, costs and success over a certain period of time [17].
After numerous clinical studies, the merits of Dr. Brennemark,
Schroeder, Strauman, and especially Dr. Zarb in the 1980s expanded
the indication area for the implantation of dental implants from the
purely toothless and toothless jaws of patients. The results of
successful oseointegration climb to more than 90 per cent, so
implantology is also experiencing a commercial boom and is accepted
as a valid therapeutic discipline [15,18,19].
This age is characterized by the emergence of new and modification
of old designs as well as the emergence of new surgical techniques.
The basis of this new philosophy consisted of oseointegration and a
number of preconditions that need to be met in order for it to be
achieved. Albrektsson et al. (1981) published educations about a
number of factors to be taken for successful oseointegration.
Oseointegration is a direct link between bone and implants, without
inserted layers. However, it does not occur to 100 per cent - the
development of bone and implant connections. Therefore, the
definition of oseointegration is based on stability, not
histological criteria, which reads "the process of achieving
clinically asymptomatic rigid fixation of aloplastic material in the
bone, during the functional load" [13.17]. Some scientists believe
that only a biomechanical factor determines whether a fibrous
capsule or bone will be created around the implant [13.18]. Contrary
to this understanding, there is well-documented evidence of how the
bone's response is quantitatively different depending on the type of
biomaterials and the roughness of its surface [13,20]. The surface
of the dental implant is the only part that is in contact with the
biological environment, and the uniqueness of the surface directs
the response and affects the mechanical strength of the contact of
the implants / tissue [20,21]. One of the main reasons for modifying
the surfaces of dental implants is the reduction of oseointegration
time. This may include mechanical treatments (for example processing
and sanding), chemical treatments (acid-etching), electrochemical
treatments (anodyne oxidation), vacuum treatments, thermal and laser
treatments. The surface layer on the implant is needed to increase
the functional surface of the bone-implant touch so that stress is
transmitted effectively. In addition, surface coating accelerates
bone aposition. The latest innovations in dental implants include
the use of fluoride, hydroxy-apathy, antibiotics, growth factors and
laminna [20,21].
In the 1990s, the concept of prosthetics guided by surgery was
replaced by the concept of prosthetic quided surgery and the focus
of interest in oral implantology shifted from functional and
aesthetic aspects. More or less, the imediate loading is replaced by
delayed. Also, procedures of bone augmentation are being introduced
to compensate for lost bone and put the implants in the correct
position. So-called tissue engineering opens up completely new
horizons in planning, but also in the performance of implant
procedures [22].
Computer-designed production methods as well as computerized
three-dimensional models are used to predict stress distribution
characteristics in the implants around the bone. In recent clinical
studies Blaschke and al. reported that dental implants made of
zirconium are an adequate alternative to titanium dental implants.
In addition to excellent aesthetic results, the authors conclude
that zirconium implants enable a degree of oseointegration and soft
tissue reaction that is better than titanium dental implants
[23,24].
MUCOINTEGRATION
As it is known, the improvement of dental implants was done to
enable optimal levels of osseointegration. However, there is another
factor that is very important, the health of soft tissue. It is well
known that for the health of the teeth, periodontal tissue is not
only important because it stabilizes the teeth, it is a barrier
between the oral cavity and the teeth. The role of soft tissue is
quite similar when it comes to implants: contact between dense soft
tissue and the surface of the abutment can act as a barrier to
protecting and preserving the fundamental crestal bone. The
anatomical characteristics of soft tissue and adjacent implants
differ from soft tissue around natural dentation. Perpendicular
collagen fibres known as Sharpey fibers bind natural teeth to
cement, while collagen fibers tend to adher for the surface of the
abutment in parallel or circular beads, which is a weaker
combination. That's why the scientific community in recent years has
been focused on improving the health of periimplant soft tissue, the
health of the papilla around the implants, changing implant
platforms, surfaces of abutments in order to better functionally
adapt soft tissue. Mucogingival surgery (Pedicle grafts, gingival
graft, free connective-tissue graft, etc.) can improve the
appearance of periimplant contours [25,26,27].
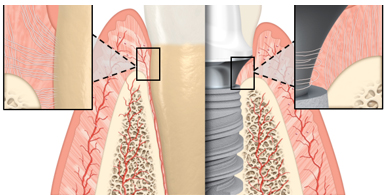
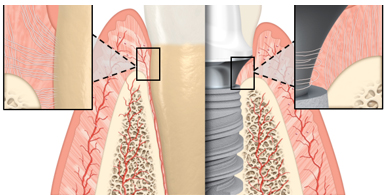
Figure 2. A comparison of the characteristics of
periodonte and periimplant soft tissue. Sharpey collagen fibers are
attached to the cement of the root of the teeth in the perpendicular
bead, while the perimplant fibers are oriented circumferentially or
parallel to the surface of the abutment. (Taken from
www.nobelbiocare.com/blog/science/why-abutment-surface-matters-for-soft-tissue-health/
for scientific purposes and not used for commercial purposes)
For long-term success, it is necessary to achieve soft tissue
stability around implants. The introduction of "prosthetic-guided
soft healing" in implant therapy aims to condition tissue before
definitive prosthetic compensation, form an optimal emergence
profile of the crown for achieving a gingive aesthetic and
complication prevention. In this concept, temporary crowns or
individualized abutments provide support to periimplantant tissues
and papillas, existing or reconstructed during the implantation
phase, ensuring positive gingive architecture without loss of volume
and vestibular recession due to the collapse of soft tissues [22].
The surface of the implant is an important factor for long-term
survival, but the role of the abutment surface has been least
examined and has been the subject of today's researchers in recent
years. As has been shown in numerous studies, smooth surface
abutments do not facilitate mechanical cleaning, but they accumulate
little plaque compared to those with rougher surfaces. Two factors
are important for soft tissue connection: nanotography and surface
chemistry [24,28,29,30,31,32]. Nanotopography of the abutment
surface becomes increasingly important in explaining the connection
between soft tissue. Surface’s nanostructure is believed to play an
important role in the interaction between cells and implants at the
cellular and protein levels [33]. There are numerous methods for
changing the nanotography of the abutment surface. One of them
prefers the method of anodization, a process that involves immersing
the abutment into electrolytic fluid using voltage. These changes in
nanotography that lead to binding and proliferation of fibroblasts
is an important step towards binding soft tissue [34,35]. The anode
process is also important for surface chemistry and energy. Research
shows that anodized surfaces have a lot of hydroxyl groups that
correlates strongly and increases hydrophilicity or affinity surface
for water, or blood [34,36]. It has also been shown that hydrophilic
surface of abutment and priorities can help with adhesia, in support
of soft tissue connection , which is functional and biological seal
and barrier and prevention of microbial colonization
[34,35,36,37,38].
There is a clear need for the abutment surface to remain clean and
intact before use, in order to achieve a protective layer through
use. Atmospheric elements can be upgraded to the surface of the
abutment even though it is in sterile packaging. These deposits tend
to have adverse effects on surface energy that are correlated with
hydrophilicity and the representation of hydroxyl groups [39,40].
When one of the world's leading implant companies, Nobel Biocare,
presented the newest surface of the Xeal abutment and together with
Ti-ultra implant surface marked the beginning of an era of
mucointegration. A smooth, non-porous, nanostructural, anodized
surface has surface chemistry and topography that is designed to
achieve soft tissue connection. Through Xeal and T-ultra Nobel
biocare, it applies the anodization process to the entire implant
system, from the abatment to the implant apex. That same year, they
promoted the "on 1" concept, which involves an interstructure,on- 1
base, which is placed on an implant in the surgical implant phase
and remains in that position during prosthetic restoration, which
minimizes soft tissue trauma. The platform is therefore transferred
from bone level to soft tissue level. Although this surface of
abutment is on the market in 2019, it is already the subject of a
two-year clinical study that showed a statistically significant
increase in the height of keratinized soft tissue compared to
machined abutments [29,41,42]. In addition to functional benefit,
its golden hue (the result of the anodyne process) is useful in
supporting natural appearance in the transmucosal zone, which can be
particularly relevant in cases where thin mucous or mucosal
recession is present. To ensure the condition of intactness,
abutments are delivered with a protective layer that dissolves after
contact with the liquid, i.e. blood. This dry packaging technology
stores the surfaces of the abutment hydrophilic and surface
chemistry and protects it from contamination with hydrocarbon [43].
DEVELOPMENT OF IMPLANT THOUGHT IN SERBIA
With the discovery of osseointegration begins the accelerated
development of implantology in the world and in our country. This is
the period when the first attempts to implantаtion in Serbia are
made. Back in 1963 Dr. Tavcar, Dr. Škokljev and Dr. Spaić at the VMA
made the first attempts to implantation two subperiostal implants in
the toothless lower jaw, but after three years they were extracted.
After the implant failure, skepticism reigned until 1977. The year
that Dr. Skundric, Dr. Spaić and Dr. Skokljev implanted
"pre-prepared wedges of a special alloy" in the form of tripods,
which in the form of tripods are attached to the bone of alveolar
continuation in the area of the canine and the first molar mutual.
At the tips of the pegs are temporary crowns of palopont filled with
silica. Encouraged by the success of the implant procedure, various
implants of foreign authors, especially leafy, needle,
screw-implants, are starting to apply in the VMA. Thanks to
Professors Perovic and Kosovcevic above all, implantology begins to
be studied in studies at the Faculty of Dentistry in Belgrade. Soon
after, in 1981 the VMA installed the first one-piece circular leaf
implant in the lower jaw [44]. Like Branemark, Schroeder, Straumann
and Zarb, Dr. Skundric in Serbia is parallelly developing the B.C.T.
home production implant system created as a product of years of
application of different systems and acquired experience. Within the
B.C.T system, this innovative scientist has also incorporated a
part, a mesostructure that irresistibly resembles what 30 years
later one of the leading implant houses, Nobel Biocare, will promote
through its concept, on-1, which marked the beginning of an era of
mucointegration.
CONCLUSION
Oseointegration is one of the most critical aspects of implant
success. The history of developing and improving dental implants is
a magnificent and fascinating time travel. In this field of research
and learning it is only possible to stop and admire man's
inventiveness over the years. Materials from which dental implants
were made range from gold ligature wire, clams, ivory to chromium,
cobalt, to iridium and platinum. From the spiral designs of
stainless steel implants to double spiral creations and endoseal
root shapes, dental researchers and clinicians worked fast and hard,
creating many structures to replace positions that once had natural
teeth. Dental surfaces have also been modified to reduce
oseointegration time. Modified surfaces include the use of
hydroxyapatites, composites, carbon, glass, ceramics and titanium
oxide. To make the exterior as convenient as possible, the surfaces
of the implants are further sanded, oxidated, fluorised, acid-etched
and modified. The latest innovative coatings are the focus of
today's implant research.
Although the importance of the surface of the implant is generally
known, the surface of the abutment is subjected to far less intense
research. Dense soft tissue contact with the surface of the abutment
can act as a barrier that protects and preserves the subcrestal bone
needed to achieve healthy integration and long-term success of
dental implants.
This was the driving factor in the development of the Xeal abutment
surface. To optimize the process of mucointegration, it is important
to understand the surface characteristics of abutment, especially
surface chemistry and nanostructure. Still the loss of implants due
to periimplantitis is a growing problem each year, so in future
aspects it should be given greater importance to soft tissue health
around implants.
REFERENCES:
- Misch, Carl E. Contemporary Implant Dentistry. St. Louis,
Missouri: Mosby Elsevier. 2007.
- Misch, C. E. Dental implant prosthetics (1st edition ed.).
St louis, Missouri 63146: Elsevier MOSBY 2005.
- Pasqualini U, Pasqualini ME. Treatise of implant dentistry:
The Italian Tribute to Modern Implantology, 2009; (1).
- Sullivan R M. Implant dentistry and the concept of
osseointegrtion: A historical perspective. J of CA Dental Assoc
2001;29 (11): 737-745.
- Twin Cities Dental Implants [homepage on the Internet].
Hopkins: Twin Cities Dental Center; c2014 [cited 2015 Aug 5].
History and types of Dental Implants. Available from:
http://www.implantmn.com/about-dental-implants/history-and-types-of-dental-implants/
- Ring M E. Pause for a moment in dental history: A thousand
years of dental implants: A definitive history - Part 1.
Compendium 1995;16:1060-1069.
- Riaud X. History of dental implantology. JBR Journal of
Interdisciplinary Medicine and Dental Sciences. 2019;2(1): 6-7.
- Caleste M A. A Brief Historical Perspective on Dental
Implants, Their Surface Coatings and Treatments. Open Dent J.
2014;16(8):50-5.
- Linkow LI, Dorfman JD. Implantology in dentistry: A brief
historical perspective. N Y State Dent J. 1991;57(6):31–5.
- Kanti Pal T. Fundamentals and history of implant dentistry.
J International Clinical Dent Research Org. 2015;(6):6-12.
- Vaidya P, Mahale S, Kale S, Patil A. Osseointegration- A
Review. IOSR-JDMS 2017; 16(1):45-48.
- Branemark R, Branemark PI, Rydevik B, Myers RR.
Osseointegration in skeletal reconstruction and rehabilitation:
A review. JRRD 2001;38(2):175-81.
- Lindhe J. Clinical periodontology and Implant Dentistry. 4th
edition. 2003; 809-820.
- Block S M. Dental Implants: The Last 100 Years. J Oral
Maxillofac Surg. 2017;76(1):11-26.
- Leney WR. In recognition of an implant pioneer: Prof.Dr.
Andre Schroeder. . Int J Oral Maxillofac Implants.
1993;8(2):135–6.
- Rajan Rajput et al. A Brief Chronological Review of Dental
Implant History. IDJSR. 2016;4(3):105-107.
- Albrektsson T, Jacobsson M. Bone-metal interface in
osseointegration. J Prosthet Dent. 1987;57:5–10.
- Brånemark PI, Zarb GA, Albrektsson T. Chicago::
Quintessence; Tissue Integrated Prostheses. 1985;201–8.
- Schroeder A, van der Zypen E, Stich H, Sutter F. The
reactions of bone. connective tissue and epithelium to endosteal
implants with titanium sprayed surfaces. J Maxillofac Surg.
1981;9:15–25.
- Sabane AV. Surface characteristics of dental implants: A
review. J Indian Acad Dental Special. 2011;2 (2):18–21.
- Alla RK, Ginjupalli K, Upadhya N, Shammas M, Rama Krishna R,
Ravichandra S. Surface roughness of implants: A review. Trends
Biomat Artif Org. 2011;25(3):112.
- Špadijer-Gostović A. Estetski izazovi u savremenoj
stomatološkoj protetici, Beograd, 2018;79-122.
- Blaschke C, Volz U. Soft and hard tissue response to
zirconium dioxide dental implants. a clinical study in man.
Neuroendocrinol Lett. 2006;27(1):69–72.
- Borotić N. Uticaj različito obrađenih površina keramičkih
abatmenata na funkcionalnu adaptaciju mekih periimplantnih tkiva.
Doktorska disertacija. 2017;5-7.
- Uike S, Gattani D and Borkar P. Soft Tissue Considerations
Around Dental Implants – A Review. SF J Oral Med Dent Health
2020; 1(1):1001.
- Gibbs S, Roffel S, Meyer M, Gasser A. Biology of soft tissue
repair: gingival epithelium in wound healing and attachment to
the tooth and abutment surface. Eur Cell Mater. 2019;38:63-78.
- Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg
B, Thomsen P. The soft tissue barrier at implants and teeth.
Clin Oral Implants 1991;(2):81-90.
- Al Rezk F, Trimpou G, Lauer HC, Weigl P, Krockow N. Response
of soft tissue to different abutment materials with different
surface topographies: a review of the literature. Gen Dent
2018;66(1):18-25.
- Hall J, Neilands J, Davies JR, et al. A randomized,
controlled, clinical study on a new titanium oxide abutment
surface for improved healing and soft tissue health. Clin
Implant Dent Relat Res 2019;21(1):55-68.
- Nosswitz M, Teale M, Mathes S, Venturato A, Gasser A.
Evaluation of anodized surfaces designed for improved soft
tissue integration. Foundation for Oral Rehabilitation (FOR)
2019;1-7.
- Quirynen M, van der Mei HC, Bollen CM, Schotte A, Marechal
M, Doornbusch GI, Naert I, Busscher HJ, van Steenberghe D. An in
vivo study of the influence of the surface roughness of implants
on the microbiology of supra- and subgingival plaque. J Dent Res
1993;72:1304-1309.
- Elter C, Heuer W, Demling A, Hannig M, Heidenblut T, Bach
FW, Stiesch-Scholz M. Supra- and subgingival biofilm formation
on implant abutments with different surface characteristics. Int
J Oral Maxillofac Implants 2008;23:327-334.
- Mendonça G., Mendonça D. B. S., Aragão F. J. L., Cooper L.
F. Advancing dental implant surface technology— from micron- to
nanotopography. Biomaterials. 2008;29(28):3822–3835.
- Guida L, Oliva A, Basile MA, Giordano M, Nastri L,
Annunziata M. Human gingival fibroblast functions are stimulated
by oxidized nanostructured titanium surfaces. J Dent.
2013;41:900-907.
- Wang X, Lu T, Wen J, et al. Selective responses of human
gingival fibroblasts and bacteria on carbon fiber reinforced
polyetheretherketone with multilevel nanostructured TiO2.
Biomaterials. 2016;83:207-218.
- Yang Y, Zhou J, Liu X, Zheng M, Yang J, Tan J. Ultraviolet
light-treated zirconia with different roughness affects function
of human gingival fibroblasts in vitro: The potential surface
modification developed from implant to abutment. J Biomed Mater
Res Part 8. 2015;1038:116-124.
- Mussano F, Genova T, Laurenti M, Zicola E, Munaron L, Rivolo
P, Mandracci P, Carossa S. Early response of fibroblasts and
epithelial cells to pink-shaded anodized dental implant
abutments: An in vitro study. Int J Oral Maxillofac Implants
2018;33:571-579.
- Rompen E, Domken O, Degidi M, et al. The effect of material
characteristics, of surface topography and of implant components
and connections on soft tissue integration: a literature review.
Clin Oral Implants Res 2006;17 (2):55-67.
- Att W, Hori N, Takeuchi M, Ouyang J, Yang Y, Anpo M, Ogawa
T. Time-dependent degradation of titanium osteoconductivity: an
implication of biological aging of implant materials.
Biomaterials. 2009;30:5352-5363.
- Hori N, Att W, Ueno T, Sato N, Yamada M, Saruwatari L,
Suzuki T, Ogawa T. Age-dependent degradation of the protein
adsorption capacity of titanium. J Dent Res. 2009;88:663-667.
- Susin C, Finger Stadler A, Fiorini T, et al. Safety and
efficacy of a novel anodized abutment on soft tissue healing in
Yucatan mini-pigs. Clin Implant Dent Relat Res 2019;21(1):34-43.
- Roffel S, Wu G, Nedeljkovic I, et al. Evaluation of a novel
oral mucosa in vitro implantation model for analysis of
molecular interactions with dental abutment surfaces. Clin
Implant Dent Relat Res 2019;21(1):25-33.
- Milleret V, Lienemann PS, Gasser A, Bauer S, Ehrbar M,
Wennerberg A. Rational design and in vitro characterization of
novel dental implant and abutment surfaces for balancing
clinical and biological needs. Clin Implant Dent Relat Res
2019;21:e15-e24.
- Todorović lJ, Lazić Z. Razvoj implantološke misli i struke
na ovim prostorima od smelih početaka do danas. Oralna
implantologija, 2001;(2): 7-11.
|
|
|
|