|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
| UDK 618.14-072.1 618.177-089 COBISS.SR-ID 46373897 |
Page 72 |
|||||||||||||||||||||||||||||||||||
|
Original paper The importance of operative hysteroscopy in treating pathologies of the uterine cavity in infertile patients Aleksandar P. Dević (1), Ana M. Dević (1), Mladenko Vasiljević (2), Goran Zajić (3) (1) CLINICAL HOSPITAL CENTER ZEMUN, OBSTETRICS AND GYNECOLOGY HOSPITAL, SERBIA; (2) OBSTETRICS AND GYNECOLOGY HOSPITAL ‘’NARODNI FRONT” BELGRADE, FACULTY OF MEDICINE, UNIVERSITY OF BELGRADE, SERBIA; (3) ACADEMY OF TECHNICAL AND ART APPLIED STUDIES – ICT COLLEGE, BELGRADE, SERBIA |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | Abstract: According
to the definition of the World Health Organization (WHO),
infertility is the inability of a sexually active, non-contracepting
couple to achieve pregnancy in one year. One of the causes of
sterility is inborn and acquired uterine anomalies. The best
visualization of the inside of the uterus is achieved
hysterscopically. Hysteroscopy is a minimally invasive surgical
procedure and has the greatest significance in the diagnosis and
treatment of congenital anomalies of the uterus. It is possible to
eliminate and correct most of the congenital anomalies of the
uterus, and it also enables the removal of other pathological
changes in the cavity of the uterus. The incidence of congenital
uterine anomalies in general population is 0.1- 3.5%. Infertile
patients have a higher incidence of these anomalies which range from
3-6%, and 5-10% in habitual abortions. The study included 200
infertile patients up to 40 years of age, with performed surgical
hysteroscopy due to diagnosed changes in the uterine cavity. The
patients were operated at the Department of infertility of the
Obstetrics and Gynecology Clinic "Narodni Front" in Belgrade, in
2013. and 2014. The following pathological changes of the uterine
cavity, were hysteroscopically removed: submucosal fibroids type 0
and type I. The aim of this paper was to evaluate the success of
operative hysteroscopy in the treatment of pathological changes of
the uterine cavity in infertile patients, based on the number of
relapses in the first six months upon surgery. Relapses occurred in
0.5% of patients during a six-month postoperative course.
Complications during hysteroscopic operations were intraoperative
and postoperative. There were 1.5% of overall complications in the
participants. Keywords: infertility, hysteroscopy, submucosal fibroids. …………….. The paper presents the most significant results of the subspecialist paper “The importance of operative hysterscopy in treating pathologies of the uterine cavity in infertile patients”, authored by Dr Aleksandar P. Dević under the mentorship of Prof. Mladenko Vasiljević. |
|||||||||||||||||||||||||||||||||||
INTRODUCTIONHysteroscopy is a minimally invasive surgical procedure which is of the greatest importance in the diagnosis and treatment of congenital uterine anomalies [1,2]. Hysteroscopic examination is usually performed in the first phase of the menstrual cycle [3]. Hysteroscopy can also be done regardless of the phase of the menstrual cycle if the patient has been previously prepared with oral contraceptives [4]. Hysteroscopy can be diagnostic and operative [5,6]. After hysteroscopic surgeries the fertility rate is significantly improved, as well as the overall percentage of pregnancies and live births, whereas the rate of miscarriages significantly decreases in these patients [7,8]. In our country, the total frequency of infertility is around 15%. The most frequent uterine causes of infertility are congenital anomalies of the uterus and uterine fibroids [9]. The significance of fibroids as the cause of infertility is even greater now due to an increasing number of women who decide to give birth later in life, at the time when uterine fibroids are more frequent [10,11]. The accepted parameters for fibroids being the cause of infertility are the following: subserosal fibroids that are ≥5 cm in diameter, intramural fibroids that are 2-3 cm in diameter and submucosal fibroids that are 1-2 cm in diameter [12]. It has been proven that the percentage of pregnancies and implantations is significantly lower in patients with intramural and submucosal fibroids even when there is no cavum deformity [13]. The percentage of pregnancies upon myomectomy is up to 60% [14,15]. THE AIMThe aim of the paper was to assess the success of operative hysteroscopy in treating pathological changes of the uterine cavity caused by fibroids in infertile patients taking into consideration the number of relapses in the first six months upon surgery and the number of intraoperative and postoperative complications. THE MATERIAL AND METHODThe research included 200 infertile patients of up to 40 years of age who had been previously diagnosed with fibroids in the uterine cavity and thus had an operative hysteroscopy done for removing the fibroids. The patients were randomly selected and they were all operated on during 2013. and 2014. at the Obstetrics and gynecology hospital "Narodni front". A rigid hysteroscope with an outer sheath 9 mm in diameter and a resectoscope containing a bipolar electrode for resecting pathological changes in the uterine cavity was used for performing hysteroscopy [16,17]. Saline solution (0,9% NaCl) was used for the distension of the uterine cavity [18]. The following pathological changes of the uterine cavity were removed: submucosal fibroids type 0 and type I [19]. The success of hysteroscopic surgeries was assessed according to the number of relapses in the first six months upon surgery [20]. In all the patients the following parameters were analyzed: age, occupation, education, the type of infertility, the duration of infertility, the presence of previous miscarriages or labors, ultrasound findings, hysterosalpingography findings, and diagnosed fibroids in the uterine cavity. The decision to perform a hysteroscopic surgery was made according to ultrasound or hysterosalpingography findings [21]. Submucosal fibroids were classified using the European Society for Hysteroscopy’s classification as type 0 (pedunculated, i.e. completely located in the uterine cavity), type I (≤50% of the fibroid is located in the myometrium whereas its ≥ 50% is located in the uterine cavity) and type II (≥50% of the fibroid is located in the myometrium and its ≤50% is located in the uterine cavity) [19,22,23]. Hysteroscopic surgeries were performed in the first phase of the menstrual cycle between day 6 and day 12, under general endotracheal anesthesia and after adequate preoperative preparation of the patient [21,16]. The collected data were analyzed using the methods of descriptive statistics (the mean and standard deviation) and analytical statistics (Chi-square test, Mann-Whitney U test and Student’s t-test). A database was created on an ASUS X% 1 RL computer using the software package SPSS 10.0 for analyzing the data. The results obtained were presented using figures and tables and they were compared with the results obtained by other authors. According to the collected data certain conclusions were made. RESULTSIn this part the most significant results are presented through
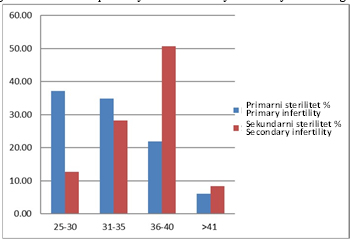
tables and figures. Figure 1 shows the distribution of primary and
secondary infertility according to the patient’s age. Figure 1. Percentage distribution of primary and secondary infertility according to the patient’s age.
There is a large statistically significant difference in the
distribution of groups formed according to age between the patients
with primary infertility and those with secondary infertility
(U=2493.5; p<0.001). Moreover, a statistically highly significant
correlation was found between the age groups and the type of
infertility (r=0.408; p<0,001), which indicates a significantly more
frequent correlation between primary infertility and older patients.
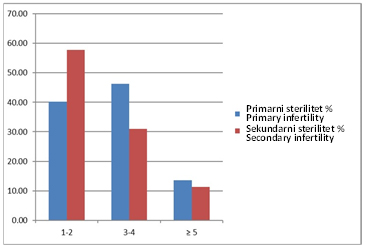
Figure 2. Percentage distribution of primary and secondary infertility according to the duration of infertility in the observed patients.
The duration of infertility in patients with primary infertility
is statistically significantly longer when compared to the patients
with secondary infertility, (U=3907.5; p<0.05). Besides, a
statistically significant correlation was found between the duration
of infertility and the type of infertility (r=0.151; p<0,05), which
indicates a significantly more frequent correlation between primary
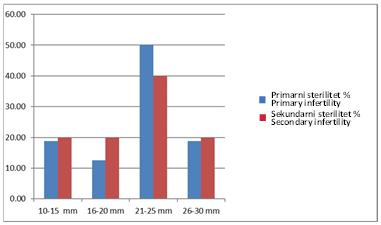
infertility and the duration of infertility. Figure 3. Percentage distribution of the size of submucosal fibroids in patients with primary and secondary infertility.
There is no statistically significant difference in the size of
submucosal fibroids between the patients with primary infertility
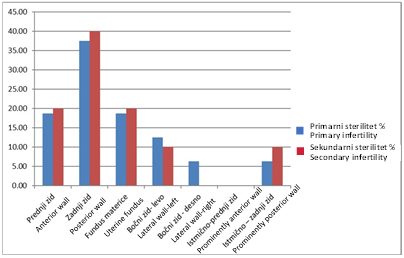
and those with secondary infertility (U=76.000; p>0.05). Figure 4. Percentage distribution of the location of submucosal fibroids in patients with primary and secondary infertility.
There is no statistically significant difference between the
patients with primary infertility and those with secondary
infertility concerning certain locations of submucosal fibroids
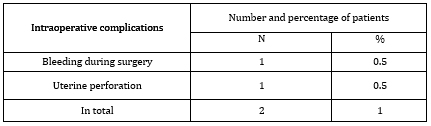
(U=76.500; p>0.05). Table 1. Intraoperative complications of hysteroscopic surgeries
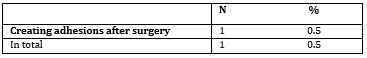
Table 2 presents the most frequent postoperative complications of hysteroscopic surgeries.
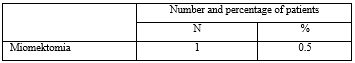
Table 3 presents the frequncy of relapses in the first six months upon a hysteroscopic surgery of fibroids.
Six months upon a hysteroscopic surgical myomectomy there was a relapse in one patient, p>0.05. DISCUSSIONObserving the type of infertility in relation with
the age of the examined patients, we found that primary infertility
was approximately equally represented in patients of 25-30 years of
age and those of 31-35 years of age, whereas secondary infertility
was most often represented in patients of 36-40 years of age. In
most of our patients, primary infertility lasted for 3-4 years,
while secondary infertility lasted for 1-2 years. Transvaginal
ultrasound is accurate in diagnosing uterine fibroids [23,24]. No
abnormalities were found in 10.6% of the patients. There is no
statistically significant difference when it comes to individual
locations of submucosal fibroids between the patients with primary
and secondary infertility and there is no significant difference
concerning the size of submucosal fibroids between these two groups
of patients [25]. CONCLUSIONHysteroscopy is a safe and efficient endoscopic procedure for diagnosis and surgical removal of submucosal fibroids as one of the factors causing pathological conditions of the uterine cavity. Submucosal fibroids which deform the uterine cavity reduce a woman’s fertility. Submucosal fibroids type 0 and type I 21-25 mm in size located on the dorsal wall of the uterine corpus were most often resected using the hysteroscopic procedure. The percentage of intraoperative complications was 1%. One patient experienced perforation of the uterus and one patient had uterine bleeding. The percentage of postoperative complications was 0.5%. One patient experienced adhesion formation in the uterus after fibroid resection. The percentage of relapses six months upon surgery was 0.5% as one patient had a relapse of a submucosal fibroid. Through adequate planning and performance it is possible to minimize the risk of complications during hysteroscopic surgeries. Advantages of the hysteroscopic approach include a shorter procedure, a better observation of the cavity, a greater precision, less pain, lower morbidity, the absence of cuts, faster recovery and getting back to work sooner. REFERENCES:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
|
Corresponding Address: Aleksandar P. Dević, Kliničko bolnički centar Zemun, Bolnica za ginekologiju i akušerstvo, Srbija E-mail: anavjestica74@gmail.com |
Paper received: 8.6.2021 Paper Internet issues: 23.9.2021 |
|||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||