| |
|
|
INTRODUCTION
Ankle fractures are relatively common, with an incidence of 187
fractures in 100,000 (1: 800) people per year [1], i.e. comprising
3.92% of all fractures in the body [2]. Posterior malleolus
fractures are very common, comprising between 7% to 44% of all ankle
fractures [3,4]; and are very rare on their own, and this is a
fracture of the Volkmann triangle [5]. Ankle is a supporting joint
in the human body, and fractures generally occur within rotation of
the body with the foot fixed in different positions. Destot [6] was
the first who described posterior malleolus in 1911, and Henderson
[7] was the first who introduced the term trimaleolar fracture in
1932. Trimaleolar ankle fractures have a poorer prognosis than
injuries without posterior malleolus fractures, so-called
bimalleolar fractures [8,9] - fractured displacement, disorder of
articular surfaces congruence, tibiotalar subluxation and
instability of the ankle joint occure in this situation.The aim of
ankle joint fracture treatment is to reduce and restrain talus in
its anatomical position and inserting it into the ankle fork.
Posterior malleolus is a very important structure in the distal
tibiofibular joint - providing restriction for distal fibula and
stabilizing tibiofibular syndesmosis via posterior inferior
tibiofibular ligament (PITFL) and inferior transvers ligament (ITL).
Ogilvie-Harris et al. [10] state that PITFL enables 42% of strength
and stability of syndesmosis. Integrity of the posterior malleolus
and ligamentous adhesions is important for weight transfer,
posterior talus stability, and rotational stability. This type of
ankle joint fracture is associated with posterior tuberculum tibia
fracture, to which the PITFL is attached.
Indications for internal fixation of posterior malleolus fracture
depend on size and degree of fragment dislocation. Lateral
radiography is used for fracture diagnostics, although computerized
tomography (CT) is increasingly recommended. If the fragment
comprises more than 25% of tibial ceiling and there is a dislocation
larger than 2mm, then there is instability of ankle joint with
associated syndesmosis injury, and persistent posterior talus
subluxation – in this case there exists an absolute indication for
surgery [11,12]. The images are also used to determine the angle
between bimaleolar axis and posterior malleolus fracture line, up to
40°, representing the degree of external tibia rotation [12].
The posterior malleolus needs to be fixed for a number of reasons:
it forms a part of articular tibia surface, with a fracture there
occurs articular non-congruence of the ankle joint, contact pressure
between joint surfaces is disrupted - the larger the fragment is,
the larger the pressure [13]. Due to the attachment of PITFL from
fibula to posterior malleolus, the non-fixed posterior malleolus
eventually leads to secondary fibula dislocation, even though it is
fixed, which creates a possibility for postero lateral talus
instability. After reduction and posterior malleolus fixation,
articular tibia surface is restored, fibula is not shortened,
syndesmosis is stable and the patient's rehabilitation is faster
[14].
Ankle joint fractures occure when external rotational force,
abduction or adduction are applied to the foot that is fixed in
supination (in 70% of occurence) or pronation (in 30% of occurence)
[15].
The aim of this paper is to present the role and importance of
posterios malleolus fixation during surgical treatman of trimaleolar
fractures.
MATERIAL AND METHODS
We retrospectively present a group of 21 patients who had ankle
joint fracture and were surgically treated at the Clinic for
Orthopedics and Traumatology in Niš from January 2013 to December
2015. Fixation of posterior malleolus was also performed, with a
minimum follow-up period of 18 months.
Criteria for including patients in this study are: 1) definitive
diagnosis of a ankle joint fracture based on clinical and
radiological findings, 2) fracture of posterior malleolus, 3)
posterior malleolus fragment occupies >25% of tibial joint surface,
4) the fragment is unstable and misplaced > 2mm, 5) reduction and
fixation of malleolus have been applied, 6) patients age is from 18
to 70 years, 7) complete clinical monitoring for 3,6,12 and 18
months.
Clinical and radiological examinations are necessary; post-injury
and post-surgery CT should be performed, but we did not do it.
Size of the posterior malleolus fragment was determined in LL
radiological image. It is obtained by dividing the length of distal
articular surface of tibia by the length of the fragment - this is
the distance from the fracture line to posterior edge of tibia,
expressed in %. Vertical dislocation is measured in LL image, and it
is the height of posterior tibia edge step, expressed in mm. We
measured the degree of external rotation [12] in the same image
(Figure 1).
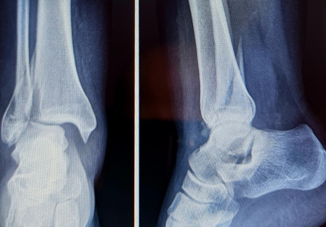
Figure 1. Antero posterior and lateral
radiographic presentation of a luxurious fracture with complete
dislocation and trimaleolar fracture
We systematized all ankle fractures according to Lauge Hansen
system [16], based on the mechanism of injury. The first word
describes foot position, and the other describes movements of talus
relative to the extremity. There are five types of ankle joint
fractures: supinational external rotational type (SER), supinational
adductional (SA), pronational external rotational (PER), pronational
abductional (PA) and pronational dorsiflexional (PD) type. The
posterior malleolus fractures most commonly occur (>70%) in SER type
of fractures in stage IV, and subsequently in PER [17,18].
Haraguchi et al. [19] provided a classification for three types of
posterior malleolus fractures.
Type I - posterior outer oblique fracture line, fragment is
wedge-shaped and includes posterior outer part of tibial ceiling;
appropriate surgical approach is posterolateral;
Type II - transversely internal fracture, the fracture line includes
tibial noch (fibula dent) down to medial malleolus, and there are
usually two fragments; appropriate surgical approach is medial or
prolonged medial, with the aim of fixing only the medial fragment
which is always larger;
Type III - small flaky fracture, that includes posterior edge of the
tibia in the form of flake; this type of fracture does not require
surgical intervention.
Having prepared the patient (early surgical intervention should be
endeavored), we immediately performed surgery in spinal or I.V.
conductive anesthesia with Tourniquet.
For direct reduction and fixation of posterior malleolus
posterolateral approach was used and the screw was placed (1 or 2)
in postero-anterior (PA) projection; we did not use the plate.
Indirect reduction was achieved after osteosynthesis of lateral and
medial malleolus with transfixation of syndesmosis; then we made an
Rtg image and determined the position of posterior malleolus - if it
is good, we place the screw in AP or PA position (Figure 2). In a
number of patients, we did not perform fragment fixation due to its
size (less than 15% of the tibia joint surface).
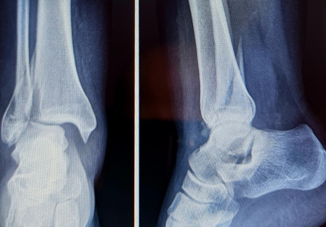
Figure 2. Antero posterior and lateral
radiographic presentation of combined osteosynthesis of posterior,
external and internal maleolus.

After the surgery, we placed a lower leg plaster orthosis for
three weeks, and after 6 weeks, we allowed the patients to walk with
crutches and lean on the treated leg, with a gradual load increase .
We perform radiological control examination after surgery in order
to check the posterior malleolus reduction, and CT scan is also
recommended. The reduction can be excellent (articular step is
<1mm), when the articular surface is flat,good (when the step is
<2mm); and poor reposition (> 2mm), when the surface is uneven [20].
We evaluated treatment results according to the Olerud-Molander
classification [21], subjective and objective signs were monitored.
Post-traumatic arthritis (PTA) was determined in Rtg images during
the follow-up of patients, and according to the following score: 0 -
normal joint, 1 - osteophytes without joint space narrowing, 2 -
joint space narrowing with or without osteophytes, 3 - joint space
disappearing and deformation (22).
RESULTS
A series of 21 operated patients was presented. There were 12
(57.1%) women and 9 (42.9%) men, 18 to 70 years old (average age
48.8). Etiological causes of fracture are: a fall at the same level
- sports, skating 11 (52.3%) patients, a fall from a height 6
(28.6%) and traffic accident 4 patients (21.1%).
The size of posterior malleolus fragment was 27,3% on the average
(25% to 34%).
Degree of external rotation, i.e. angle between the two lines was 00
to 400
According to Lauge Hansen classification, there were 15 (71,4%)
patients with fracture of type SER, 4 patients (19%) of type PER and
2 patients (9,6%) of type PA.
According to Haraguchi classification of posterior malleolus
fracture, there were 12 (57,1%) of patients witi fracture of type I,
6 patients (28,5%) of type II and 3 patients (14,4%) of type III.
Elapsed time from the moment of injury to surgery was 1,6 days (1-5
days) on the average.
Direct reduction and screw fixation was applied in 6 patients,
indirect reduction and fixation in 12, and in 3 patients a fixation
of lateral and medial malleolus was applied, and thus a reduction of
non-fixed posterior malleolus was achieved.
Postoperative direct reduction was excellent in 5 (83.3%) patients
and good in 1 (16.7%). As for indirect fragment reduction, we had
excellent results in 6 patients (50%), good in 3, and bad in another
3 (25 %). By comparing these results, it is evident that fracture
reduction quality was significantly higher in direct reduction
group, compared to the group where reduction was performed
indirectly (p = 0.039).
After follow-up period of 16 months (12 to 18 months) on the
average, we evaluated the results according to the Olerud-Molander
score. There were excellent results (91% - 100%) in 13 (61.9%)
patients, good (61% - 90%) ) in 7 (33.4%) patients, and poor (0% -
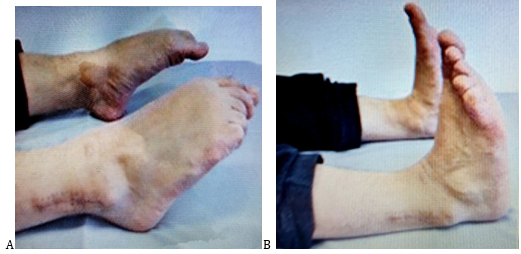
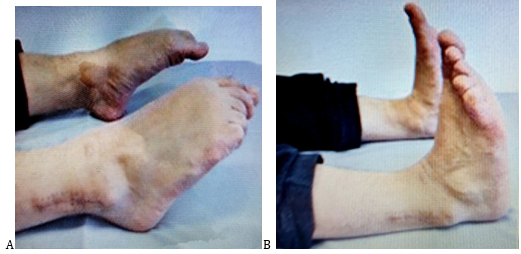
30%) in 1 (4.7%) patient (Figure 3A,B).
Figure 3. The photograph shows the anterolateral
aspect of plantar (A) and dorsal (B) flexion of the foot.
Postoperatively, superficial wound infection occurred in 2 (9.4%)
patients – it was treated with antibiotics, parenterally for 4 days,
and postoperative thrombophlebitis in 1 (4.7%) patient – it was
treated with low molecular Heparin. There were no fractured screws
and all fractures healed in up to three months.
Post-traumatic arthritis (PTA) was evaluated one year after surgery
and we obtained the following results: grade 0 in 9 (42.9%)
patients, grade 1 in 10 (47.7%) patients, and grade 2 in 2 (9.4%) )
patients - in total, 12 (57.1%) patients had PTA.
DISCUSSION
Ankle joint fractures are the third in frequency, right after hip
and wrist joint fractures. Final functional outcome is better in
bimaleolar, compared to trimalleolar fractures. They occur in young
people, and with high energy trauma (accident, fall from a height
and sport), and in elderly persons low-energy trauma causes
fractures due to osteoporosis. In young people there is a risk of
developing post-traumatic arthritis cousing changes in the quality
of life, due to a reduction of ankle joint function and chronic
pain. In elderly patients there is a risk of infection, wound
complications and fixation disintegration [11].
Ankle joint fractures are intraarticular, resulting in articular
surfaces injury, osteochondral layer disruption, joint surface
displacement, and presence of blood and bone content in the joint
[23].
From a biomechanical point of view, posterior malleolus plays a
significant role in transmission of tibiotalar load. It has a
preventive effect on posterior talus displacement, and with fragment
size, the risk of posterior talus subluxation increases, especially
if the fragment is larger than 25% of tibia joint surface [24,25].
Posterior maleolus is an important structure in distal tibiofibular
joint - it provides bone restriction to distal fibula and
syndesmosis stability via posterior inferior tibiofibular ligament (PITFL)
and inferior transversum ligament (ITL).
Ramsey et al. and Lloyd et al. [26,27] indicate great intraarticular
contact pressure in talus displacement as a result of ankle joint
injury. Talus displacement by 1mm and external fibula rotation of 3°
lead to a 40% decrease of tibiotalar contact, joint incongruence
occurs, and decrease of contact surface causes increased pressure
per unit of measurement. There is a great deal of stress that
damages articular cartilage, which is the main factor in
pathogenesis of PTA.
The goal of surgical intervention in posterior malleolus fractures
is to achieve articular congruence, to achieve stability and restore
ankle joint function. For these reasons, the imperative is to
achieve anatomic reduction, and to provide a smooth and flat
cartilage surface. Anatomical reduction of articular surfaces is
essential factor for good treatment outcome of unstable posterior
malleolus fractures [28].
Orthopedic reduction and posterior malleolus fixation can be direct
and indirect. For direct access and reduction, posterior lateral
approach is used, and lateral malleolus can be indirectly reduced
[29]. Due to a deep position of posterior malleolus and tendon-neuro-vascular
bundle of the area, this approach is very demanding and difficult.
Haraguchi et al. [19] recommend this approach for type I posterior
malleolus fracture. For type II fracture, a medially extended
approach is recommended. Fragment fixation can be direct with screws
or a plate [8]. Indirect fixation is performed by placing a screw in
AP or PA direction, but only after performing lateral and medial
malleolus osteosynthesis, and radiologically checking posterior
malleolus position [12]. In posterior malleolus type III fractures,
fragment repositioning can be achieved using the principle of
ligamentotaxis, because after lateral malleolus repositioning and
tibiofibular syndesmosis transfixation, there occurs a spontaneous
posterior malleolus reposition – it is pulled to its place by intact
PITFL [18,30]. The degree of fixation reduction and stability is the
greatest in direct reposition and with the use of an osteosynthesis
plate, and lower in indirect reposition and stabilization [31].
Huber et al. [32] report that indirect reduction and stability were
achieved in 27% cases, while it was achieved in 83% in direct
reduction and stabilization. Our results range within this frame.
Relationship and connection between posterior malleolus and
tibiofibular syndesmosis is very important because of PITFL and ITL.
These ligaments attach to fibula and posterior malleolus and are
very important distal tibiofibular joint structures, as they provide
stability to lateral ankle joint side, i.e. lateral part of talus
and fibula. If the PITFL is preserved and open reposition and
fixation of posterior malleolus is performed, syndesmosis stability
will be better than stability in case when transsyndesmal fixation
is performed. PITFL complex is the nucleus of tibiofibular
syndesmosis stability. The fracture of posterior malleolus alters
syndesmosis stability, because of the injury and loss of PITFL
function [33]. Rigid fibula fixation and posterior malleolus
reduction and fixation can adequately restore ligamentous tension of
PITFL, and stabilize syndesmosis without transsyndesmal fixation.
Gardner et al [34] found, after performing posterior malleolus
repositioning and stabilization on cadavers, that 70% of distal
tibiofibular joint stability was achieved, while after transindezmal
fixation it was 40%.
Functional outcome of ankle joint fracture associated with posterior
malleolus fracture depends on: the size of posterior malleolus
fragment, its comminution, the quality of anatomic reposition and
fixation stability, and on articular stability [18]. Our clinical
results are good and similar to those reported by other authors
[14,20,33].
A common late complication in posterior malleolus fractures is
post-traumatic arthritis (PTA). The trigger for its formation is the
change of articular surfaces, caused by trauma to distal tibia and
talus [35]. Risk factors for PTA are: residual articular
displacement, joint instability or subluxation caused by an injury,
damage on articular surfaces at the moment of injury [36]. Boist and
Dust [37] had PTA grades 2 and 3 in 67% of cases in their series,
and the results presented in our series of patients are similar to
theirs.
CONCLUSION
Posterior malleolus fractures are common in ankle injuries.
Posterior malleolus fixation is necessary if the fragment is larger
than 25% of tibial joint surface. Direct reduction and fixation
should be performed, as the results are better. Fixation restores
articular surface, PITFL and syndesmosis stability is achieved. CT
helps in classifying the fracture type, and after surgery helps in
determining the degree of fragment and joint surface reduction.
REFERENCES
- Daly PJ, Fitzgerald RH Jr, Melton LJ, Ilstrup DM.
Epidemiology of ankle fractures in Rochester, Minnesota. Acta
Orthop Scand 1987;58:539–44.
- Salai M, Dudkiewicz I, Novikov I, Amit Y, Chechick A. The
epidemic of ankle fractures in the elderly–is surgical treatment
warranted? Arch Orthop Trauma Surg. 2000;120(9):511–513.
- Court-Brown CM, McBirnie J, Wilson G. Adult ankle
fractures–an increasing problem? Acta Orthop Scand.
1998;69(1):43–47.
- Hai-lin XU, Li-min LIU, Bao-guo JIANG, et al. Multicenter
follow-up study of ankle fracture surgery. Chinese Medical
Journal. 2012;125(4):574–578.
- Neumaier Probst E, Maas R, Meenen NM. Isolated fracture of
the posterolateral tibial lip (Volkmann's triangle) Acta Radiol.
1997;38(3):359–362.
- Destot E. Traumatismes du poignet et rayons
X.Paris:Masson;1911;109-134.
- Henderson MS.Trimalleolar fractures of the ancle.Surg Clin
North Am.1932;12:86
- Anwar A, Zhang Z, Lv D, Lv G, Zhao Z, Wang Y, Cai Y, Qasim
W, Nazir MU, Lu M. Biomechanical efficacy of AP, PA lag screws
and posterior plating for fixation of posterior malleolar
fractures: a three dimensional finite element study. BMC
Musculoskelet Disord. 2018; 19: 73.
- Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S.
Management of Posterior Malleolar Fractures: A Systematic
Review. J Foot Ankle Surg. 2016;55(1):140-5.
- Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the
ankle syndesmosis: biomechanical study of the ligamentous
restraints. Arthroscopy. 1994;10:558–560.
- Duan X, Kadakia AR. Operative Treatment of Posterior
Malleolar Fractures. Open Orthop J. 2017;11:732-742.
- Naoki H, Hiroki H, Hidekazu T, Fumio K. Pathoanatomy of
posterior malleolar fractures of ankle. J Bone Joint Surg
Am.2006;88:1085-1092.
- Hartford JM, Gorczyca JT, McNamara JL, Mayor MB. Tibiotalar
contact area. Contribution of posterior malleolus and deltoid
ligament. Clin Orthop Relat Res 1995;320:182–187.
- Solan MC, Sakellariou A. Posterior malleolus fractures:
worth fixing. Bone Joint J. 2017;99-B(11):1413-1419.
- Vasileios Lampridis, Nikolaos Gougoulias, and Anthony
Sakellario. Stability in ankle fractures.Diagnosis and
treatment. EFORT Open Rev. 2018; 3(5): 294–303.
- Lauge Hansen N. Ligamentous ankle fractures.Diagnosis and
treatment. Acta Chir Scand 1949; 97: 544 – 50.
- Xing W, Wang Y, Sun L, Wang L, Kong Z, Zhang C, Zhang Z.
Ankle joint dislocation treating dislocated trimalleolar
fractures accompanied with the complex posterior malleolus
fracture without separation of the tibiofibular
syndesmosis.Medicine (Baltimore). 2018;97(37):e12079.
- Fitzpatrick DC,Otto JK,McKinley TO,Brown TD.Kinematic and
contact stress analysis of posterior malleolus fractures of the
ancle. J Orthop Trauma.2004;18:271-8.
- Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of
posterior malleolar fractures of the ankle. J Bone Joint Surg
[Am] 2006;88-A:1085–1092.
- Xu HL, Li X, Zhang DY, Fu ZG, Wang TB, Zhang PX, Jiang BG,
Shen HL, Wang G, Wang GL, Wu XB. PurposeA retrospective study of
posterior malleolus fractures. Int Orthop. 2012;36(9):1929-36.
- Olerud C, Molander H. A scoring scale for symptom evaluation
after ankle fracture. Arch Orthop Trauma Surg 1984;103:190-4.
- Domsic RT, Saltzman CL. Ankle osteoarthritis scale. Foot
Ankle Int 1998;19:466–71.
- Olson SA, Furman B, Guilak F. Joint injury and
post-traumatic arthritis. HSS J. 2012;8(1):23-5.
- McDaniel WJ, Wilson FC. Trimalleolar fractures of the ankle.
An end result study. Clin Orthop Relat Res. 1977;122:37–45.
- De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. Long-term
results of ankle fractures with a posterior malleolar fragment.
J Foot Ankle Surg. 2005;44:211–217.
- Ramsey PL, Hamilton W. Changes in tibiotalar area of contact
caused by lateral talar shift. J. Bone Joint Surg. Am.
1976;58:356–357.
- Lloyd J, Elsayed S, Hariharan K, Tanaka H. Revisiting the
concept of talar shift in ankle fractures. Foot Ankle Int.
2006;27:793–796.
- Gougoulias N, Khanna A, Sakellariou A, Maffulli N.
Supination-External Rotation Ankle Fractures: Stability a Key
Issue. Clin Orthop Relat Res. 2010; 468(1): 243–251.
- Talbot M, Steenblock TR, Cole PA. Posterolateral approach
for open reduction and internal fixation of trimalleolar ankle
fractures. Can J Surg. 2005;48(6):487-90.
- Mak KH, Chan KM, Leung PC. Ankle fracture treated with the
AO principle-an experience with 116 cases. Injury.
1985;16(4):265–72.
- OʼConnor TJ, Mueller B, Ly TV, Jacobson AR, Nelson ER, Cole
PA. "A to p" screw versus posterolateral plate for posterior
malleolus fixation in trimalleolar ankle fractures. J Orthop
Trauma. 2015;29(4):e151-6.
- Huber M, Stutz PM, Gerber C. Open reduction and internal
fixation of the posterior malleolus with a posterior antiglide
plate using a postero-lateral approach-a preliminary report.
Foot Ankle Surg. 1996;2(2):95–103.
- Bilgehan Tosun, Ozgur Selek, Umit Gok, and Halil Ceylan.
Posterior Malleolus Fractures in Trimalleolar Ankle Fractures:
Malleolus versus Transyndesmal Fixation.Indian J Orthop. 2018;
52(3): 309–314.
- Gardner MJ, Brodsky A, Briggs SM, Nielson JH, Lorich DG.
Fixation of posterior malleolar fractures provides greater
syndesmotic stability. Clin Orthop Relat Res. 2006;447:165-71.
- van den Bekerom MP, Haverkamp D, Kloen P. Biomechanical and
clinical evaluation of posterior malleolar fractures. A
systematic review of the literature. J Trauma 2009;66:279–84.
- Anderson DD, et al. Is elevated contact stress predictive of
post-traumatic osteoarthritis for imprecisely reduced tibial
plafond fractures? J Orthop Res. 2011;29(1):33–9.
- Bois AJ, Dust W. Posterior fracture dislocation of the
ankle: Technique and clinical experience using a posteromedial
surgical approach. J Orthop Trauma. 2008;22:629–36.
|
|
|
|