|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
Page 137 |
||||||||||||||||||||||||||||||||||||
|
Case report Hashimoto encephalopathy with positive oligoclonal bands in cerebrospinal fluid Vesna Martić (1), Aleksandar Stojanov (2), Tihomir Ilić (3) (1) CLINIC OF NEUROLOGY MILITARY MEDICAL ACADEMY, BELGRADE, SERBIA; (2) CLINIC OF NEUROLOGY, CLINICAL CENTER OF NIS, NIS, SERBIA; (3) MEDICAL UNIVERSITY MILITARY MEDICAL ACADEMY, BELGRADE, SERBIA |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | Abstract:
Introduction: Hashimoto encephalopathy (HE) is a rare and often
misdiagnosed entity. Except high levels of the thyroid peroxidase
(anti-TPO) and antithyroglobulin (anti-TG) antibodies,
neurophysiological and psychological tests are beneficial for the
diagnosis. The presence of oligoclonal bands in the cerebrospinal
fluid (CSF) of these patients is very rare. We present a patient
with HE and oligoclonal bands in CSF with good clinical response on
corticosteroid therapy. Case report: Male patient, 39 years old,
suddenly developed focal neurologic deficit. He had elevated anti–TPO
and anti TG antibodies, impaired concentration on psychologist
report and oligoclonal bands in CSF. Slowing of
electroencephalography activity was normalized with full clinical
recovery of the patients, after corticosteroid therapy. The patient
is in clinical remission 5 years after establishing the diagnosis. Conclusion: Oligoclonal bands in the CSF may be helpful in the diagnosis of HE considering that it is still poorly understood entity. Also fast diagnosis of HE and treatment with corticosteroids are important for a full recovery of this patients. Key words: Hashimoto encephalopathy, cerebrospinal fluid, oligoclonal bands |
|||||||||||||||||||||||||||||||||||
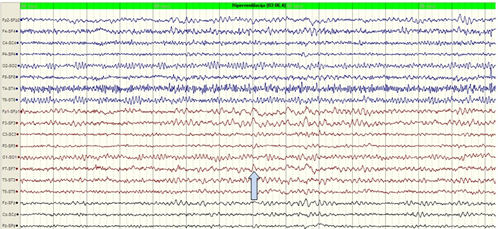
INTRODUCTIONHashimoto encephalopathy (HE) is a cerebral disorder in patients with autoimmune disease of the thyroid gland [1]. The first case of HE with high serum concentrations of thyroid peroxidase (anti-TPO) and antithyreoglobulin (anti-TG) antibodies, thyroiditis, cognitive decline and tremor was described by Brain in 1966 [2]. It is known today that prevalence of this disorder is 2/100 000, with female predominance (gender ratio 4:1). HE usually begins in 5th or 6th decade of life [3]. Possible clinical manifestation of HE are cognitive impairment, psychiatric manifestation (confusion, interference with memory, alteration of consciousness from somnolence to coma, amnesia, psychotic symptoms), seizures, focal neurological deficits, movement disorders, headache [4]. HE is considered as a vacuities of cerebral small blood vessels. This is supported by perivascular lymphocytic inflammation in the brain tissue, presence of unknown pathogenic autoantibodies and immune complexes in some HE patients, specific astrocyte binding of anti-TPO antibodies, and good response to steroid treatment as a hallmark of the diagnosis [5]. The presence of oligoclonal bands in cerebrospinal fluid is reported in only few HE cases [6]. We present a case of a patient with HE and oligoclonal bands in cerebrospinal fluid (CSF) with a good recovery after corticosteroid therapy. CASE REPORTMale, 39 years old, patient was hospitalized as an emergency case due to transitory confusion and aphasia (developed suddenly) with later amnesia for that period. He was normotensive with normal cardiac status and with normal neurological status at the time of hospitalization. Multislice scanner angiography was normal. On electroencephalography (EEG) performed on the same day, intermittent delta-theta activity in left frontotemporal part of the brain was registered (Figure 1). There was spontaneous and nearly complete recovery of speech disturbances next day, but difficulty in the nomination and confusion persisted. Magnetic resonance imaging of his head and carotid duplex ultrasound, made on the second day, were normal. The patient had headaches, concentration and memory disturbances and elevated anti –TPO antibodies in the last few years, although he has had normal thyroid hormonal status all the time. Figure 1. EEG on the first day of hospitalization: during hyperventilation theta (about 6 Hz) and delta (2-3 Hz) activity over left frontotemporal region.
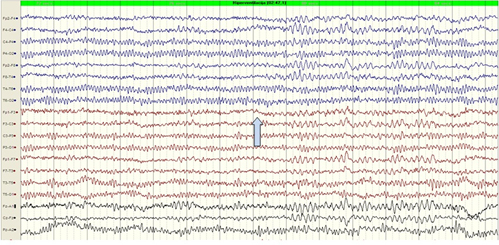
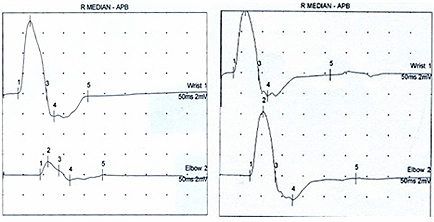
In laboratory findings during hospitalization high values of anti-TPO 127.2 IU/ml (0.0-5.7) and the anti-TG 1405.47 IU/ml (0.0-4.11) were noted, followed by normal values of the thyroid hormones and normal remaining laboratory findings. In CSF protein content of 0.58 g/l (0.15 – 0.45), albumin coefficient of 7.79 (up 5.7) with positive oligoclonal band was present. Report of a clinical psychologist showed neither cognitive decline efficiency nor cognitive dysfunction, but concentration was impaired. Due to the subjective feeling of weakness in his right arm nerve conduction study (NCS) was performed, and conduction block of the median nerve in his right cubital region was detected. Spontaneous recovery on the control EEG was registered (intermittent theta activity over the temporal regions in both hemispheres) (Figure 2). Figure 2. EEG after spontaneous resolution of speech problems, and before starting corticosteroids in the treatment: the intermittent activation of the HV 6-7 Hz bilaterally
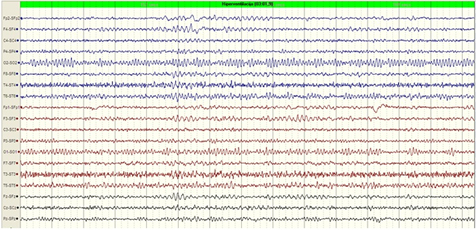
We also performed some additional tests such as: CSF cultures, autoimmune workup, drugs screen. All of the results were normal. Based on previously mentioned findings, the diagnosis of HE was established in this patient and he was treated with three-day pulsed corticosteroid therapy (500 mg daily, iv) followed by alternative oral corticosteroid therapy during next 6 months. Headache reduced significantly and finally stopped, and there were no confusion and speech disturbances after start of the therapy. Clinical recovery was monitored, supported by neurophysiological recovery recorded on the EEG (Figure 3) and NCS (Figure 4.). No new clinical symptoms or signs in next 7 years were reported. Figure 3. EEG done after completed corticosteroid therapy: during hyperventilation no change in the basic activities
Figure 4. Conduction block of the median nerve and normal findings after several months of corticosteroid therapy
DISCUSSIONHE is a very rare, poorly understood and often misdiagnosed
entity. Abnormal elevations of thyroid antibodies are required for
HE diagnosis: anti-TPO in all patients and anti-TG in half of them
[7]. In the present patient, both antibodies were multiplied more
than hundred times, but he had no pathologic findings of thyroid
hormones at the time of diagnosis. It is interesting that initial
higher serum TPO antibodies titers are associated with more
satisfactory outcomes [8]. However, as high titer of plasma anti-TG
antibodies has been detected in patients with B hepatitis, C
hepatitis, in patients with type 1 diabetes and Helicobacter pylori
infection, specificity of plasma anti-TG antibodies in HE diagnosis
is low [9]. Except presence of high titer of anti-TPO antibodies and
clinical manifestation, there are no well-established diagnostic
criteria for HE, so HE is a diagnosis of exclusion. A broad list of
differential diagnoses must be kept in mind and ruled out (e.g toxic
metabolic encephalopathies, meningoencephalitis, psychiatric
disease, stroke, drug abuse etc). In our patient tumor markers, drug
screening, laboratory of his blood and CSF and radiological brain
exploration exclude other disorders considered important in
differential diagnosis. LITERATURE:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||