| |
|
|
Introduction According to experiences from previous
epidemics and pandemics of infectious diseases around the world,
restrictive epidemiological measures in the form of restriction of
movement, social isolation and distancing and prevention of physical
contact, although effective in reducing transmission and infection
rates, cause a state of increased collective psychological tension,
fear (1-3). The most stressful aspects of such public health crises
are their unpredictability, as well as uncertainty regarding disease
control and assessment of the degree and severity of health risks.
Uncertainty, constant challenges and stress in crisis situations
such as epidemics and pandemics of infectious diseases can
negatively affect mental disorders by inducing them and complicating
their course and outcome (4).
The SARS-CoV-2 virus pandemic itself as well as all epidemiological
measures introduced to curb it pose a psychological burden on the
population, disrupting the personal, family and social functioning
of the individual, especially in vulnerable social groups such as
psychiatric patients, margins of society (5).
The negative consequences of the SARS-CoV-2 virus pandemic on the
mental health of the population around the world are already
visible. According to expert estimates, they will reach their peak
in the coming period and will very likely survive the current
pandemic for a long time (6). Research by Brooks et al points out
that periods of self-isolation, restrictions on social contacts and
quarantine, even shorter than 10 days, can have long-term
consequences with the presence of mental disorders up to 3 years
later (7).
Studies have appeared primarily by Chinese authors that note the
negative impact of the SARS-CoV-2 viral pandemic on mental health,
and especially on the growing anxiety and depression among Chinese
health workers, in the general population, but also in the group of
psychiatric patients.
Therefore, this study aims to compare the mental health effects of
the SARS-CoV-2 viral pandemic on patients with psychiatric illness
compared to previously mentally healthy individuals, and thus to
contribute to the general knowledge of the overall consequences of
SARS-CoV-2 viral pandemic.
Material and methods
The study is designed as a cross-sectional study. It was
conducted during May and June 2020 at the end and immediately after
the first wave of the SARS-CoV-2 viral pandemic in Serbia.
Participants were divided into two groups - a clinical group of
patients with mental disorders and a control group composed of the
general population who had no previous mental disorders.
Participants for the clinical group were recruited within the
outpatient-specialist psychiatric service, and for the control
group, students filled out the same questionnaire in online form.
The basic criterion for inclusion of subjects in the clinical group
was the presence of a mental disorder from before, while the control
group was composed of selected subjects without pre-existing mental
disorder. Data were collected through a specially designed
questionnaire for self-assessment of the existence and intensity of
mental symptoms in respondents. The questionnaire first contained a
set of general questions about sociodemographic characteristics and
the previous existence of a psychiatric disorder. Then, questions
were created about the existence of fear, mental tension,
irritability, anxiety, the appearance of panic attacks, and the
overall level of anxiety and feelings of uncertainty. Then there
follows a series of questions that aim to record the symptoms from
the depressive spectrum, especially with reference to anhedonia,
loss of emotions, pleasure, the appearance of feelings of sadness
and depression. Then there is the question of sleep and sleep
problems as the symptom that is most indicative of the appearance of
a certain psychological distress. There are also direct questions
about suicidal thoughts and intentions. The main reason for the
generalized feeling of fear and uncertainty are questions about the
fear of losing a job, poverty and misery, and a possible decline in
the quality of life due to material difficulties that arose during
the SARS-CoV-2 viral pandemic. Also, the unavailability of adequate
health care due to the state of emergency and restrictive measures
was stated as a contributing factor of uncertainty and concern. As a
form of self-help and human defense mechanisms against the current
stressful situation, the need for the use / increased use / abuse of
psychopharmaceuticals is assumed, and on the other hand, man's
attempt to improve his lifestyle and overcome the crisis by his own
efforts and struggles. The SPSS for Windows 20 program, which runs
under the Microsoft Windows environment, was used for data
processing. The results are shown tabularly.
In order to compare the group of respondents with mental disorders
and those without a diagnosis in terms of sociodemographic
characteristics and questions from the questionnaire on mental
disorders, the χ² test was applied.In addition to the statistical
significance, the differences in the prevalence of individual
psychological symptoms among the examined groups in this study were
compared semiquantitatively according to the following scale:
frequency up to 10% was considered insignificant, 11% to 20% was
considered moderate, and 21% to 40% % of frequency of psychological
symptoms was considered high, while frequency of over 41% was
determined to be extremely high.
Results
A total of 200 subjects participated in the study, half of whom
had a mental disorder, while the other half of the subjects had no
mental disorders.
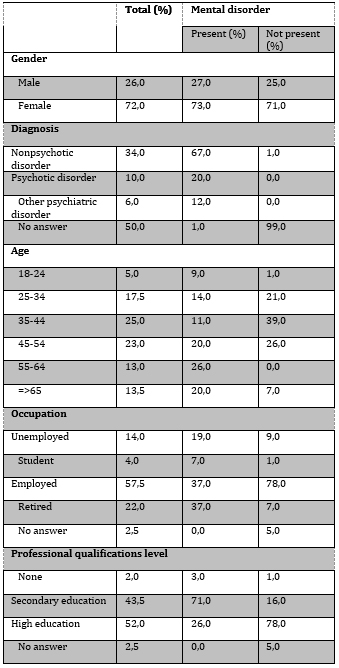
Table 1. Sociodemographic characteristics on the
whole sample (N = 200) and according to the presence of a mental
disorder
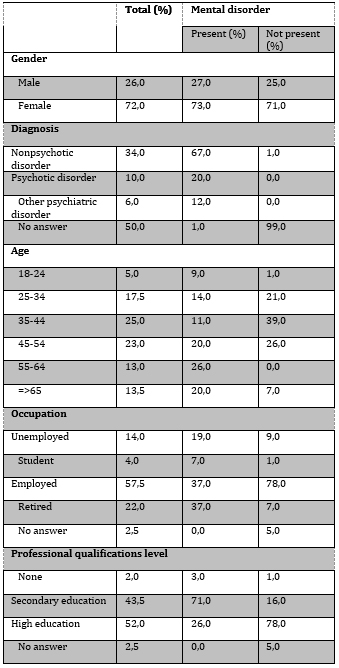
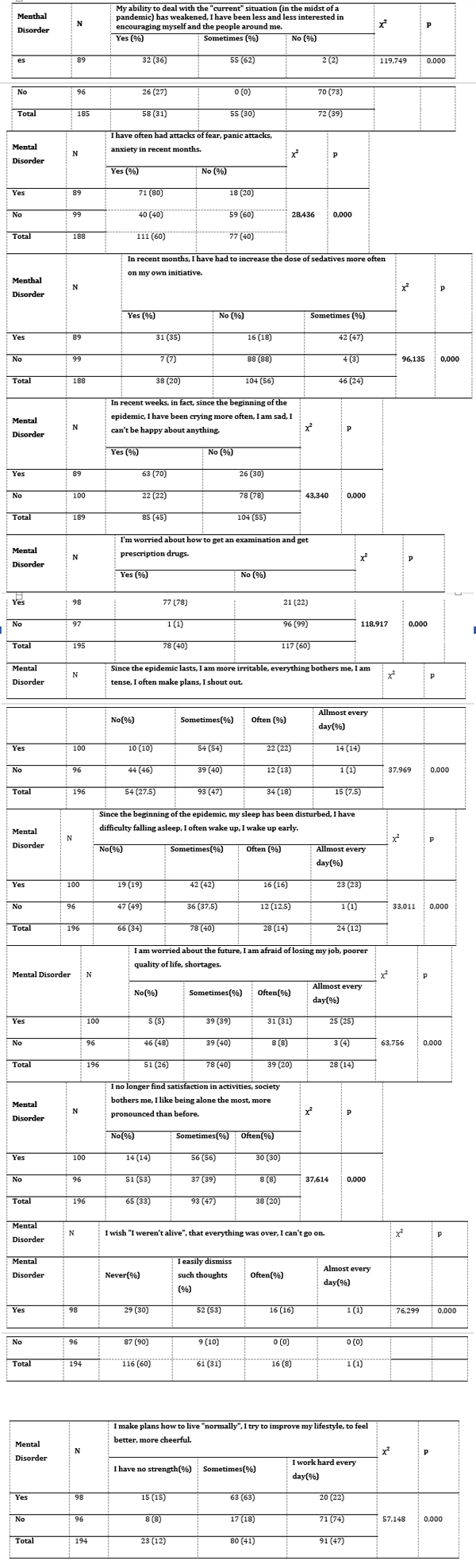
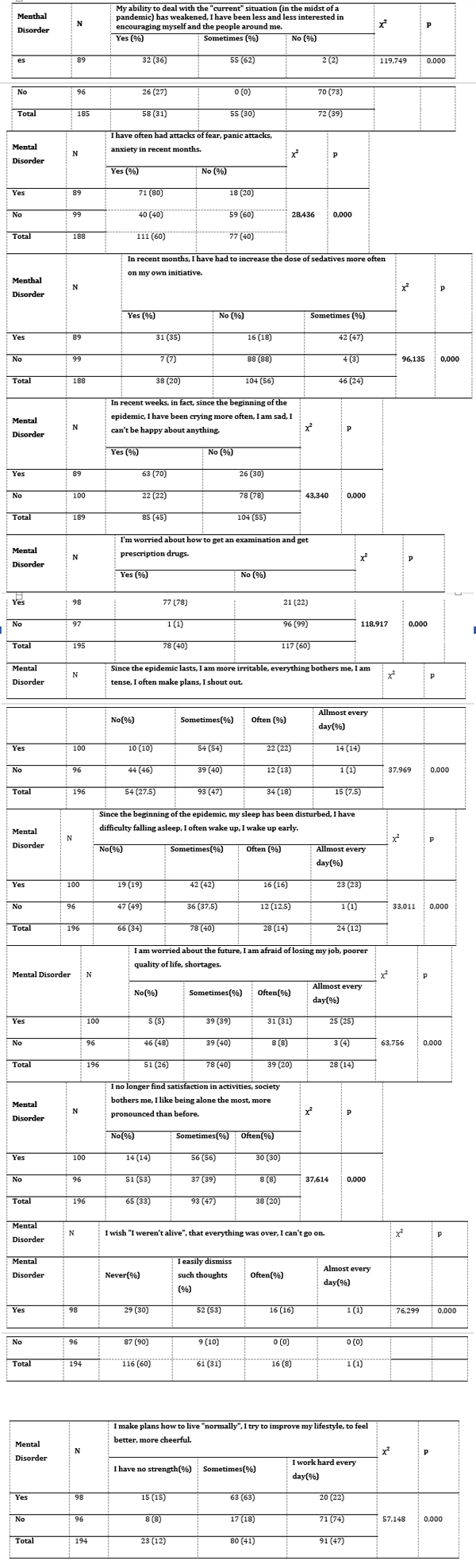
Table 2. Comparison of two groups of respondents
(with and without mental disorders) regarding the questions from the
questionnaire on mental state
Discussion
The aim of this study was to compare the state of mental health
in psychiatric patients with previously mentally healthy people
during and after the first wave of the SARS-CoV-2 viral pandemic in
Serbia. The results of this study suggest that all the observed
symptoms are far more frequent and more pronounced in the population
of patients previously suffering from psychiatric diseases compared
to healthy subjects. Anxiety-depressive symptoms dominate in the
form of more frequent panic attacks, feelings of inability to cope
with the current crisis situation, irritability, tension and
constant worries about the future regarding their own health and
uncertain financial situation and future quality of life, and
feelings of loss of satisfaction and depressed mood. Then there is
the concern about the lack of adequate health care during curfews
and lockdowns, and self-initiated use / abuse of
psychopharmaceuticals. Also, problems with sleep and sleep in the
form of insomnia, difficulty falling asleep, intermittent and easy
sleep are much more common in the group of mentally ill people.
Also, the presence of suicidal thoughts is also more common in
subjects with mental disorders. Among the respondents from general
population without pre-existing mental disorder, ie. among the
respondents from the control group there was a statistically
significantly lower presence of symptoms and signs related to mental
problems, although in this group the percentage of symptoms of
mental disorders is not negligible (anxiety, fear, panic attacks
(40%), depressive symptoms. However, this group of respondents (92%)
is of the opinion that it is necessary to fight to overcome the
current crisis, to do their best to “live normally, feel happier and
better. Despite all the hardships and troubles, these results show a
significantly higher incidence of anxiety and depressive symptoms
among the general population in Serbia compared to most similar
studies around the world related to the first outbreak of the
SARS-CoV-2 virus pandemic Namely, the percentage of anxiety and
depression among general population during the first attack of the
SARS-CoV-2 virus pandemic is 26% and 17% in China, 21% and 18% in
Italy, 22% and 19% in Spain, and Saudi Arabia and 24% and 29%
(8-11). This discrepancy in the results between our and world
studies is a consequence of cultural differences, but also of the
efficiency of the public health authorities of our country in
suppressing the first wave of the epidemic, but also in the
strictest measures to suppress the epidemic, such as state of
emergency and total social restriction.
In the initial wave of the SARS-CoV-2 viral pandemic in Serbia,
there were no more than 400 infected per day and the mortality rate
was up to 1%. With timely public health intervention, the epidemic
was effectively and relatively quickly contained (12).However, the
strictest epidemiological measures, such as the absolute ban on
movement during the state of emergency in our country, have left a
significant mark on the mental health of the general population,
which is reflected in significantly higher rates of tension, anxiety
and fear among our general population which are almost twice as high
than in European countries such as Italy and Spain, and the
countries of the Middle and Far East such as Saudi Arabia and China.
The rate of depression among the general population is within the
world average.
On the other hand, paradoxically, all these factors have contributed
to the majority of the healthy population mobilizing their defense
mechanisms, to awaken empathy, care for the general safety and
health of vulnerable groups of people. Morality and fighting spirit
were at the highest level, and therefore the psychopathological
phenomena examined were not significantly examined, but the values
obtained are by no means negligible, especially in terms of the
frequency of anxiety.Most people have found additional sources of
psychic energy and strength to cope with a stressful situation and
not succumb to psychopathological manifestations in the first place
(13). Taking the above into account, it can be expected that the
most pronounced effects of a pandemic on mental health in the
general population will be visible only after the situation has
calmed down, when the overstretched healthy defense mechanisms in
humans subside, for which high prevalence of fear, anxiety and
tension among the general population are a sure pre-sign. Patients
with mental illness certainly represent a vulnerable social group
that is particularly sensitive to each new crisis and stressful
situation, which further worsens their already fragile mental
health.This was once again confirmed by the results of our study.
Certainly, the capacities for healthy overcoming of crisis
situations due to mental illness in patients with psychiatric
disorders have been reduced. The results of our study support such
attitudes. For psychiatric patients, social interactions of crucial
importance for their rehabilitation are of particular importance.
And as quarantine and physical distancing measures are in place in a
pandemic, psychiatric patients are prevented from continuing with
daily group rehabilitation treatments and therapeutic group
activities. Such circumstances often leave psychiatric patients
alone with enough time to ruminate their psychopathological
contents, which inevitably manifests itself through anxiety and
tension, and a depressed mood with all its other correlates (14). In
addition to the general feeling of fear and uncertainty, among
psychiatric patients, there is a particular concern about the
availability of medical care in terms of prescribing drugs that
patients use regularly. Namely, over three quarters of the
participants in the study with a mental disorder stated that they
were concerned about the availability of doctors and medical care,
especially in terms of prescribing prescriptions for
psychopharmaceuticals. In our study, respondents (statistically
significantly increased number of former psychiatric patients)
stated that due to growing anxiety and worry, they need to increase
the dose of tranquilizers on their own initiative. From these facts,
a clear conclusion follows that most psychopharmaceuticals were
procured illegally, without a doctor's prescription, which is still
possible in our country. Although it is also clear that the word is
primarily about benzodiazepines, as the most common sedatives and
sleeping pills. A study by Chinese authors, on the other hand, notes
that a significant number of psychiatric patients stopped using
psychopharmaceuticals during the epidemic, because it was not
possible to obtain them through a doctor's prescription (15). As
around the world, there are several reasons in Serbia for mental
health care to be relegated to the background. In the first place,
of course, is the care for the physical health due to the SARS-CoV-2
viral pandemic and the protection of the population from infectious
diseases. Also, health systems have largely reoriented themselves to
providing assistance to patients with Covid 19. All other patients,
including psychiatric ones, have been advised not to see the doctor
unnecessarily, in order to reduce the pressure on the health system.
On the other hand, the patients themselves avoided visiting the
doctor for fear of becoming infected (16). Emergency psychiatric
care was also provided to a much lesser extent both in Serbia and
around the world, as evidenced by the results of a study by Italian
authors (17). Regarding suicide in the first wave of the SARS-CoV-2
viral pandemic , according to the results of our study in the total
sample, about a third of the respondents had suicidal thoughts.
There is a statistically significant difference in the two examined
groups in relation to the occurrence of sicidal thoughts. Far more
respondents of psychiatric patients (approximately 66%) in the
conditions of the SARS-CoV-2 viral pandemic, stated that on a number
of occasions they thought of taking their own lives. For the sake of
comparison, in the control group of mentally healthy people, the
rate of suicidal thoughts is about 9%. Certainly, the frequency of
suicidal ideation correlates positively with the increase in the
intensity of mental symptoms in the group of psychiatric patients
compared to mentally healthy controls. There is little data on
suicide rates at the time of the SARS-CoV-2 viral pandemic . The
data available to us are from a study by authors from Bangladesh
where it is stated that the incidence rate of suicidal thoughts and
thinking in the general population is about 6% at the beginning of
the SARS-CoV-2 viral pandemic (18). In this study, as well in as
several others, loneliness, social isolation, depressed mood, and
fear are highlighted as leading risk factors for suicidal ideation
and attempts. The most susceptible to such phenomena are medical
workers who participate in the treatment of infected patients, but
also the infected patients themselves (19,20). In European
countries, there has been a significant decline in the number of
suicides during the first "lockdown" period, according to prominent
news agencies, although these data still need to be scientifically
substantiated (20).There are no clear data in the world regarding
the occurrence of suicide in psychiatric patients at the time of the
SARS-CoV-2 viral pandemic. Most authors who touch on this topic only
state that the presence of a mental disorder and the SARS-CoV-2
viral pandemic represent "double-susceptibility" to suicide (21).
Suicide rates are expected to decrease during the stressful
situation of a large number of people as they focus on maintaining
both their own health and the health of others (22). Only after the
action of the stress factor, after the defense mechanisms have
subsided, does a person turn to thinking about himself and his own
re-examination, which is a suitable ground for the appearance of
suicidal thoughts and behaviors.
Conclusion. We found that the SARS-CoV-2 viral pandemic after its
first outbreak in Serbia left double consequences on the mental
health of the healthy population and those previously suffering from
psychiatric illnesses. Namely, psychiatric patients responded to the
first wave of the SARS-CoV-2 viral pandemic and all the restrictive
measures that followed it with a significant worsening of
psychopathological symptoms. Anxiety and depressive symptoms, as
well as sleep disorders, but also the presence of suicidal thoughts
and thoughts are mostly recorded. While, on the other hand, mentally
healthy participants in the control group had a statistically
significantly lower presence of symptoms and signs associated with
mental problems, although in this group the percentage of symptoms
of mental disorders is not negligible, which supports the thesis
that mental retardation The CoV-2 virus brought with it, especially
in the long run, leads to serious mental disorders, which is
predicted by world experts in the field of mental health (7).These
results clearly show once again that psychiatric patients represent
a vulnerable social group, whose mental health should not be
neglected under any circumstances, and especially in stressful
situations such as the SARS-CoV-2 viral pandemic . Our findings can
be used to plan public health interventions in the field of mental
health targeting both general and vulnerable populations combined
with efforts to respond to certain future pandemics in their early
stages, with the aim of to obtain a comprehensive response in which
even mental health will not be neglected. Limitations of the study
This study may be limited by its design (cross-sectional study), as
well as the method of data collection (independent and online
completion of self-assessment questionnaires), also by the fact that
standardized psychiatric-psychological questionnaires were not used
to assess mental health. It is possible to assess the intensity of
psychopathological symptoms. These limitations may methodologically
weaken the study. However, despite the possible limitations of the
study, it provides new and interesting data on different
psychological responses to the SARS-CoV-2 viral pandemic in two
groups of people who are different by the presence/absence of a
mental disorder, and is therefore unique in the area, wherethere is
a lack of information on global level.
LITERATURE:
- Maunder R, Hunter J, Vicent L, Bennett J, Peladeau N, Leszcz
M, et al. The immediate psychological and occupational impact of
the 2003 SARS outbreak in a teaching hospital. CMAJ
2003;168:1245–51.
- Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term
psychiatric morbidities among SARS survivors. Gen. Hosp.
Psychiatry. 2009;31, 318–26.
- Van der Weerd W, Timmermans DR, Beaujean DJ, Oudhoff J, van
Steenbergen
JE. Monitoring the level of government trust, risk perception
and intention of the
general public to adopt protective measures during the influenza
A (H1N1) pandemic
in the Netherlands. BMC Public Health. 2011;11:575. doi:
10.1186/1471-2458-11-575.
- Dar KA, Iqbal N, Mushtaq A. Intolerance of uncertainty,
depression, and anxiety: examining the indirect and moderating
effects of worry. Asian J. Psychiatr. 2017;29, 129–33.
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al.
Impact of COVID-19 pandemic on mental health in the general
population: A systematic review. J Affect Disord.
2020;1(277):55-64.
- Pietrabissa G, Simpson SG. Psychological Consequences of
Social Isolation During COVID-19 Outbreak. Front. Psychol. 2020;
11:2201.
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S,
Greenberg N. The psychological impact of quarantine and how to
reduce it: rapid review of the evidence. Lancet Psychiatry.
2020; 395(10227): 912–20.
- González-Sanguino C, Ausín B, Ángel Castellanos M, Saiz J,
López-Gómez A, et al. "Mental health consequences during the
initial stage of the 2020 Coronavirus pandemic (COVID-19) in
Spain." Brain Behavior and Immunity 2020;87:172-176. doi:
10.1016/j.bbi.2020.05.040.
- Zhou J, Liu L, Xue P, Yang X, Tang T. "Mental health
response to the COVID-19 outbreak in China." Am J Psychiatry.
2020; 177(7): 574-575. doi: 10.1176/appi.ajp.2020.20030304.
- Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS,
Aljohani MS. The psychological impact of COVID-19 pandemic on
the general population of Saudi Arabia. Comprehensive
Psychiatry. 2020;102:152192.
- Rossi R, Socci V, Talevi D, Mensi S, Niolu C. et al.
COVID-19 Pandemic and Lockdown Measures Impact on Mental Health
Among the General Population in Italy. Frontiers in Psychiatry,
2020;11:790. doi: 10.3389/fpsyt.2020.00790.
- Objave centra za javno zdravlje – COVID-19. Available from:
https://covid19.rs/objave-centra-za-javno-zdravlje/ [cited 2
December 2020].
- Mental Health and the Covid-19 Pandemic | NEJM [Internet].
New England Journal of Medicine. Available from:
https://www.nejm.org/doi/full/10.1056/NEJMp2008017 [cited 2
December 2020].
- Neelam K, Duddu V, Anyim N, Neelam J, Lewis S. Pandemics and
pre-existing mental illness: A systematic review and
meta-analysis Available from:
https://www.sciencedirect.com/science/article/pii/S2666354620301423
[cited 2020 Dec10].
- Zhou J, Liu L, Xue P, Yang X, Tang X. Mental health response
to the COVID-19 outbreak in China. Am J Psychiatry
2020;177(7):574-575. doi: 10.1176/appi.ajp.2020.20030304.
- Hao F, Tan W, Jiang L, Zhang L, Zhao X. et al. Do
psychiatric patients experience more psychiatric symptoms during
COVID-19 pandemic and lockdown? A case-control study with
service and research implications for immunopsychiatry. Brain
behavior and immunity. 2020;87:100-106. doi:
10.1016/j.bbi.2020.04.069.
- Capuzzi E, Di Brita C, Caldiroli A, et al. Psychiatric
emergency care during Coronavirus 2019 (COVID 19) pandemic
lockdown: results from a Department of Mental Health and
Addiction of northern Italy. Psychiatry Res. 2020;293:113463.
- Mamun MA, Akter T, Zohra F, Sakib N, Bhuiyan AKMI, Banik PC,
et al. Prevalence and risk factors of COVID-19 suicidal behavior
in Bangladeshi population: are healthcare professionals at
greater risk? 2020;6(10):e05259. Available from:
https://www.sciencedirect.com/science/article/pii/S2405844020321022
[cited 2020Dec10].
- Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and
coronavirus disease 2019—a perfect storm? JAMA Psychiatry. 2020.
- Banerjee D., Vaishnav M., Rao T.S., Raju M.S.V.K., Dalal
P.K., Javed A., Saha G., Mishra K.K., Kumar V., Jagiwala M.P.
Impact of the COVID-19 pandemic on psychosocial health and
well-being in South-Asian (World Psychiatric Association zone
16) countries: A systematic and advocacy review from the Indian
Psychiatric Society. Indian J. Psychiatry. 2020;62(9):343.
- Banerjee D, Kosagisharaf JR, Sathyanarayana Rao TS. 'The
dual pandemic' of suicide and COVID-19: A biopsychosocial
narrative of risks and prevention. Psychiatry Res.
2021;295:113577. doi: 10.1016/j.psychres.2020.113577.
- Yao H., Chen J.H., Xu Y.F. Patients with mental health
disorders in the COVID-19 epidemic. Lancet Psychiatry.
2020;7(4):e21.
|
|
|
|