|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
Page 169 |
||||||||||||||||||||||||||||||||||||
|
Review article Testicular torsion: specifics of bimodal clinical presentation, diagnosis and treatment Zorica Jovanović (1), Andjelka Slavković (1), Goran Janković (1), Maja Zečević (8), Milan Slavković (2) (1) CLINIC FOR PEDIATRIC SURGERY UNIVERSITY CLINICAL CENTER NIS; (2) UNIVERSITY CHILDREN'S CLINIC |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | Abstract: Testicular
torsion (TT) is a condition caused by twisting of the spermatic
cord, which leads to interruption of blood flow to the testicles. It
most often occurs in two different periods of growth and
development. It is significantly rarer around birth, before or
immediately after, including the first month of life, and much more
frequent at the age of 12-18. In addition to age, the
pathoanatomical substrate, mechanism of occurrence and clinical
presentation are different. In younger adolescents, it is an urgent
clinical condition, while in newborns it is usually not. The aim of
this paper is to point out these specifics, because the therapeutic
approach depends on timely recognition, which can be essentially
different. Key words: testis, torsion, adolescents, perinatal testicular torsion |
|||||||||||||||||||||||||||||||||||
|
INTRODUCTION Embryonic development of the testis begins very
early, already in the 6th week of gestation, with condensation of
the urogenital ridge tissue. In the last trimester of pregnancy, as
a result of fetal growth and under the influence of endocrine
stimuli, the testis leaves the abdomen and descends into the scrotum
through the inguinal canal. Along the way, it is followed by the
processus vaginalis, the peritoneal perversion. The testis is fixed
in the scrotum by the gubernaculum. The spermatic cord into which
the a.testicularis, plexus pampiniformis, and ductus deferens enter
occupy an inguinal position proximal to the testis. Since time is a
crucial factor in rescuing a torque testis, a good knowledge of
anatomy and embryonic development is very important in understanding
the pathophysiological mechanism of this condition [2-5]. Testicular torsion (TT) is a condition caused by twisting of the
spermatic cord, which leads to interruption of blood flow to the
testicles. Testicular tissue cannot survive without blood flow, and
loss of the affected testicle can occur if not treated immediately.
That is why TT is an urgent surgical condition and the most common
cause of testicular loss. TT can occur at any age, but most frequently in the age group of
12 to 18 years (puberty) and in the first year of life (12%). On
average, 3.8 per 100,000 men under the age of 18 have TT annually,
and it is bilateral in 40% of cases [3]. Testicular torsion is the
cause in 26% of acute scrotum and in 42% it ends with orchiectomy
[3,6,7]. 10% of boys with confirmed TT have a positive family
history [6]. The seasonal incidence of testicular torsion ranges
from 36.2% in spring, 31% in winter, 19% in summer to 13.8% in
autumn. In 81% of cases, torsion occurs when the atmospheric
temperature is lower than 15C [7]. It can also occur after physical
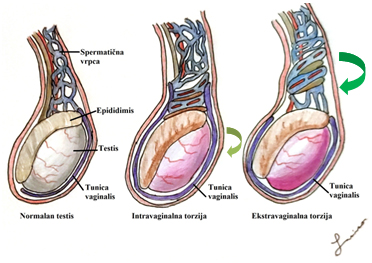
activity. The distribution by age is bimodal, as is the pathoanatomical
substrate. Extravaginal torsion occurs in fetuses and newborns,
because the testes can rotate freely before their fixation through
the tunica vaginalis inside the scrotum (Figure 1). It is usually
diagnosed in the first 7-10 days of life. Normal testicular
suspension ensures a firm fixation of the epididymal-testicular
complex on the back and effectively prevents the twisting of the
spermatic cord. Figure 1. Anatomical types of TT
Figure 2. Torsion of the mesorchium
In adolescents and men who have high attachment of the tunica vaginalis, as well as abnormal fixation of the muscular and fascial sheath, the testis can rotate freely within the tunica vaginalis (intravaginal torsion of the testis) (Figure 1). (Bell clapper), can cause the longitudinal axis of the testis to be oriented transversely, not cephalocaudally. Testis torsion can also occur if there is an abnormal mesorchium between the testis and the epididymis, when the testicle is wider than the mesentery [8 ] long mesorchium (intravaginal torsion), a rare form, which may explain the ultrasound finding of epididymal hyperemia despite scanty vascular vascularization. (Figure 2) TT IN THE ADOLESCENT PERIOD Testicular torsion is a clinical diagnosis. The clinical presentation of torsion in this age group is characterized by: unbearable unilateral pain in the affected testis, (more often on the left) with sudden swelling because the structures twist (like a puppet on a wire) and the testicle rises. Patients may have fever, nausea and vomiting, abdominal pain, and a history of previous testicular pain. If the patient has an acute scrotum in the clinical presentation, the main goal is to exclude testicular torsion, because it is the only urgent surgical condition [9]. Very often, boys cannot accurately and precisely explain the onset of symptoms, as well as their severityseriousness and duration. Many patients do not come immediately, after the onset of symptoms, further limiting the therapeutic space for testicular rescue [10]. In the anamnesis, some of the patients mention recent trauma or physical exertion, which preceded the difficulties [11]. Some also have nonspecific urinary disorders. High testicular position is indicative of twisted and shortened spermatic cord [12]. It is not of scrotal or testicular origin. For that reason, every adolescent who complains of abdominal pain should undergo an examination of the external genitalia in order to exclude the possibility of scrotal pathology. A retrospective analysis of 73 adolescent patients (mean age 15.3 years) who underwent surgical treatment of testicular torsion showed that patients who had abdominal pain, compared with patients with initial testicular pain, had a significant delay in diagnosis / treatment (mean pain duration of 36 hours versus 5 hours) Figure 3. Acute scrotum – horizontal position of the right testis
and significantly higher testicular loss rate (81% vs. 4%) [13].
The results of the study suggest that every 10 minutes in delay
reduces the chance of testicular survival by 4.8%.
Patients are classified as low-risk, medium-risk, or high-risk. The TWIST score is based on the sum, ranging from 0 to 7. The results of risk stratification for those with low risk of testicular torsion are 0 to 2 points; medium risk, 3 to 4 points; and high risk, 5 to 7 points Figure 4. Cremasteric reflex
Stimulation of the inner side of the thigh stimulates the sensory
fibres of the genitofemoral and ilioinguinal nerve when the
cremaster muscles contract with the resulting elevation of the
ipsilateral testis. (Figure 4) The consequences of testicular
torsion are: loss of spermatogenesis within 4-6 hours and loss of
hormonal function 10-12 hours after occlusion of testicular blood
vessels. Survival of the testicles after torsion is very difficult
to predict. The papers publish the survival rate if surgery is
performed in the first 6 hours after the onset of symptoms 90-100%,
and from 6-12 hours, it drops to 50%, and is less than 10% if the
symptoms last longer than 24 hours [14]. Survival of the testes
after prolonged torsion may indicate that testicular blood flow has
not been completely interrupted or that it is intermittent torsion.
Therefore, if there is a high degree of suspicion of testicular
torsion based on the anamnesis and physical examination, imaging
examinations do not have to be performed, but the patient
immediately undergoes surgical intervention. Delay in additional
diagnostics prolongs the time of testicular ischemia and reduces the
survival rate of the testis [14]. In obscure cases Doppler
echosonography, which is highly sensitive 88.8% and specific 98.8%,
with only 1% false results is used [15]. Testicular torsion
treatment: The definitive way of treating testicular torsion is
operative, after possible manual derotation. The procedure of manual
derotation of the testicles enables the relief of pain, if it is
successful, but after that the renewal of the blood flow must be
confirmed. Other signs that indicate successful manual
detoxification are: change of testicular position from transverse to
longitudinal orientation, lower testicular position in scrotum and
return of normal arterial pulsations on Doppler ultrasonography.
Subsequent orchidopexy is recommended to prevent recurrence of
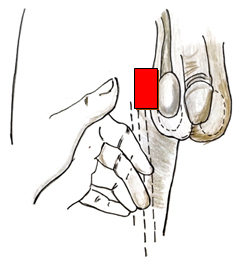
torsion. Figure 5 Manual derotation
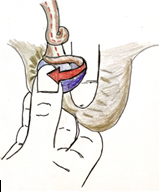
Figure 6. The direction of testicular derotation — like opening a book For manual detorquation of the torsion of the right testicle, the doctor is placed in front of the patient who is standing or lying on his back and with the left thumb and forefinger he is holding the patient's right testicle. The doctor then rotates the right testicle outward 180 ° in the medial-lateral direction. (Fig. 5) For the patient's left testicle, the doctor uses the patient's right thumb and forefinger and rotates the patient's left testicle outward 180 ° from medial to lateral. Inward and toward the midline; therefore, manual testicular derotation involves twisting outward and laterally. (Figure 6) In one series of 104 patients, lateral rotation was found in 46% of patients, and there were no factors that would indicate the direction of torsion with certainty. Figure 7. TT 360 degrees.
Figure 8. Detorned, vital testis, after 4h
In older boys with TT, the contralateral bell clapper anomaly is highly prevalent, which supports the standard practice of contralateral testicular fixation in these situations. Fixation remains a matter of the surgeon's personal preference, but the use of an absorbable suture for fixation is associated with recurrence of torsion and should be avoided [20]. Figure 9. Gangrena testis-TT after 4 days
PERINATAL TESTICULAR TORSION - PTT Torsion of the spermatic cord of the fetus and newborn is a
special and rare entity, different from the one seen in boys in
juvenile and adulthood. Testicular torsion occurs prenatally (in the
last trimester) or postnatally, in the first thirty days of life.
Taylor 1897.g. first described neonatal extravaginal unilateral
testicular torsion in the newborn. Papadatos and Moutsouris in 1967
were the first to describe bilateral testicular torsion [21]. The
symptomatology is atypical and the clinical presentation is varied.
70% develop before birth and in 30% of boys after birth. The
representation of parties is equal [22], and in 20% PTT is
bilateral, occurring more often simultaneously, but also
asynchronously [23]. Lack of consensus in diagnosis and treatment
contributes to confusion and can result in numerous medical (and
legal!) problems. Figure 10. Male newborn, twenty days old, admitted due to tumefaction in the right scrotum. Clinically and ultrasound evaluated right testis more voluminous, in the lower half hypoechoic and inhomogeneous. No free fluid in the scrotal sac Forms and time of appearance of PTT
Bilateral asynchronous TT: Since the tunica vaginalis is only firmly attached to the scrotal wallat the end of the first or second month, this period is critical for asynchronous torsion. It is important to point out that in the early prenatal period, a few weeks before birth and a few days before birth, there are no signs of inflammation, while a few hours before birth and during the first month of life, signs of inflammation are present. Unlike in adults, PTT has an insidious presentation. There are huge variations in the clinical finding depending on when the torsion occurred and when the clinical presentation was initiated. Excluding boys in whom testicular torsion occurs in the first month of life, it is often not possible to determine exactly when PTT actually occurred [31]! Differential diagnosis in the neonatal period: hydrocele, hematocele (consequence of birth trauma, adrenal hemorrhage), trapped inguinal hernia, testicular and paratesticular tumors, scrotal edema, scrotal hematoma, scrotal abscess, meconial peritonitis, epididymitis ... In the literature, there are controversies of surgical therapy in relation to: fetally verified testicular torsion, necessity of surgical exploration, urgency of surgery, place of incision (inguinal / scrotal), treatment of contralateral testis, orchiectomy, nubbin testis. There are several published papers on prenatally ultrasound-detected PTT, but with a hitherto unclear implication for therapy. Urgent fetal extraction would be justified in the last week of pregnancy if bilateral PTT is suspected, provided the diagnosis is made shortly after torsion. There have been no published papers about it yet! The question is whether postnatal TT should be operated on, and if so, when? Immediately, to delay, or not to operate. There are three possibilities: observation, elective (delayed) operation or urgent operation. Surgical variants include: urgent exploration without / with orchiectomy and contralateral testicular fixation, elective exploration with / without contralateral testicular fixation, or an exploitative posture. Reasons for exploration: The diagnosis of testicular torsion is assumed, but not always certain, the possibility of testicular preservation is small, but it is possible. If the testicle is necrotic, devitalized tissue should be removed. There are also medical and legal aspects. Kaplan and Silber [32] state that even if a prompt diagnosis and exploration is done, only about 5% of the testes can be saved, while Sorensen indicates that this percentage is 40 to 50 [33]. The explanation given by Das and Singer points out that 30% of PTT is in the postnatal period, which gives the urgent surgical approach importance in the possible rescue of the torque testicle [22]. Unilateral PTT is less controversial because it is against exploration if the possibility of testicular rescue is assessed in relation to the potential risk of emergency anesthesia and surgery in the neonatal period [30]. Many authors believe that only bilateral perinatal torsion requires urgent surgical intervention due to the risk of anarchy [34]. A study of a limited group of pediatric urologists indicates that 10% of pediatric urologists prefer urgent exploration, 57% delayed, 33% only observation [30]. The favoured approach is the scrotal incision, justified in emergency interventions [27]. Inguinal incision is justified, in the case of other (possible!) Differential diagnoses (hernias, tumors, undescended testis). Figure 11:Through a scrotal incision, the torqued right testicle was approached; torsion by 720º, “counter-clockwise”. Testicular recovery after detorsion is partial.
Do you fix the contralateral testis? With intravaginal torsion, there is an anatomical predisposition that torsion of the testicles will also occur on the contralateral side. Extravaginal torsion is a consequence of the lack of fixation of the scrotum and the vaginal tunic [36]. Recommendation: NO contralateral orchidopexy in postnatal unilateral testicular torsion, YES in adult TT because the mechanism of occurrence is different. Only one monorchid man with subsequent intravaginal torsion after postnatal torsion has been described in the literature [37]. Is orchiectomy justified / necessary? Bleeding during incision of the tunica albugina may be the best prognostic sign of potential gonadal vitality. Leaving the ischemic testis in situ, according to many authors, has no consequences for later fertility as in torsion in postpubertal men [38]. Immature spermatogenetic elements are not adequate antigenic stimulation during the neonatal period [39]. The left gonad in situ has both an aesthetic and a psychological role [40]. As there are no data on tumors arising from microscopic foci of viable testicular tissue in the nodular (nubbin) testis, there are disagreements about the preventive removal of such testicular remains [46]. 15% of the nubbin testis has seminiferous tubules. CONCLUSION A pediatric surgeon / urologist must be consulted immediately in
case of an abnormal scrotal appearance! The degree of testicular
preservation is directly dependent on the duration of symptoms. With
a correct and timely approach, it is possible to increase the
preservation rate of the affected testicle. A clear distinction
should be made between prenatal ("old") and postnatal torsion of
acute TT. Only this last group has a chance of preserving the
testicles by urgent surgical exploration.
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||