| |
|
|
1. INTRODUCTION
Malignant laryngeal tumors are among the most common tumors that
affect the upper aerodigestive tract [1,2]. It is important to point
out that they make 1-3% of all malignant tumors in human body, and
20% i.e., 25-35% of all malignant tumors of head and neck in
general, where Serbia and its region Vojvodina report one of the
greatest incidences in Europe [3,4]. One also needs to emphasize
that it is 8 to 10 times more common in men than in women, occurring
most likely at the age from 61 to 70 [4,5,6,7]. The outcome of the
treatment and patient survival rate mostly depend on the stage of
the tumor at the time when it is discovered [8]. However,
recognition of malignant laryngeal tumors in late, advanced stage is
common, despite the symptoms being present and visible even in the
early stage [3,9]. Total laryngectomy is a radical and most
comprehensive surgery of malignant laryngeal tumors that is applied
for advanced stages of the disease, and involves complete removal of
the larynx [2,10]. In physiological phonation, the role of the voice
activator is performed by lungs. After the total laryngectomy,
breathing is performed directly through the created permanent
tracheostoma. Larynx i.e., its part – glottis, represents the voice
generator, so it is obvious that the removal of the same will
disable the phonation, and the change in the anatomical organization
and separation of the activator from the resonator will also
contribute to the change in resonance, because besides the larynx,
it also depends on pharynx, nasal and oral cavity, but the trachea
itself and the lungs [4,11]. The integral part of the treatment of
patients with malignant laryngeal growths is certainly the voice and
speech rehabilitation i.e., mastering any form of alaryngeal
communication. It is important to point out the significance of the
speech rehabilitation of these patients which does not only lead to
the improvement of the communicational aspects, but also the
psychological, social, emotional and professional ones [12,13].
There are three main rehabilitation methods; esophageal voice and
speech education, surgical implantation of voice prosthesis with the
development of the tracheoesophageal voice and speech and the use of
electrolarynx [4,14,15]. The most humane, economically most
justified, and according to many authors, also the first method of
choice in rehabilitation of totally laryngectomized patients is the
use of esophageal voice and speech [4,16]. In esophageal voice, the
air, placed in the upper third of the esophagus, is used as an
activator and therefore, when acquiring it, it is most important to
ensure the functional capacity of this air reservoir, as well as the
functionality of the pharyngoesophageal segment (PE), acting as the
new glottis/pseudo-glottis [12]. In esophageal voice and speech, the
voice generator i.e., pseudo-glottis, is created on the same
vibrational segment as in the tracheoesophageal voice and speech
after the implantation of the speech prosthesis, and the difference
between them is the place and the force of the activator; in
esophageal voice it is the air in the esophagus whose volume is far
smaller, while in the tracheoesophageal voice the activator is still
the airstream from the lungs as in physiological phonation [4,12].
Besides the advantages of the esophageal voice and speech that
definitely reflect in independency of prosthetic aids, free hands,
economic cost-effectiveness and inconspicuousness by the
environment, it is also necessary to mention the deficiencies which
mostly relate to the duration of education, lower success rate,
discontinuity and insufficient intensity of speech in noisy
environments, very small air volumes that may be deposited in
esophagus (not more than 60-70 ml), with somewhat worse melody,
short duration of phrases and poorer comprehensibility of sounds
from the group of nasal consonants [6,15,17]. In developed countries
around the world, the most often used method for voice and speech
rehabilitation in laryngectomized patients is the implantation of
voice prosthesis as the gold standard in voice and speech
rehabilitation in laryngectomized patients [18]. Voice prosthesis
implantation in developed countries is most often primary i.e., in
the same act with laryngectomy, while in the developing countries,
with more patients with advanced laryngeal carcinoma and often
financial inability to provide primary implantation of vocal
prostheses, it is most often implanted secondarily, after an
unsuccessful esophageal voice and speech education [13].
The objective of this paper was to investigate the factors that may
affect the success of the esophageal voice and speech education in
clinical practice around the world and in our region, obtained from
the available literature data, as well as to point out the
significance of observing them during vocal rehabilitation of
laryngectomized patients, in order to further improve this
rehabilitation method.
2. METHODS OF WORK
Comprehensive review of the literature was performed by using the
following databases: Google Scholar, SCIndex, PubMed and
ResearchGate. The search was based on the following terminology:
laryngectomy, esophageal speech, education, factors, success,
treatment outcome, and their counterparts in Serbian language, with
focus on the most recent references available. This paper was
created by using 30 sources, mostly research scientific papers, as
well as a few professional books, meta-analyses, PhD theses but also
one final paper.
3. RESULTS
3.1. Success of the Esophageal Voice and Speech Education
As there are no clear objective and subjective criteria for
assessing the success rate of esophageal voice and speech,
consequently a very wide range of success rates of this method of
rehabilitation can be found in the literature. According to
Stanković, the success rate is 86.1% [7], Krejović Trivić et al.
[19] report similar rate - 86.3%, while according to Frith et al.
[20], this percentage is much smaller and is only 25%. Gates [21]
shares the opinion with the previously mentioned author, pointing
out that the real picture of the success of education in this type
of alaryngeal communication ranges from 26% to 34%. In her PhD
thesis, Dragičević [4] states that 66.7% of patients achieve
adequate esophageal speech.
3.2. Factors That May Affect the Esophageal Voice and Speech
Education
Different data can be found in the literature about the factors that
may affect the success of the esophageal voice and speech education.
Namely, Salmon et al.[22] group them as psychosocial and
anatomic-physiologic, where the distinction occurs within these as
well, into those that are positive and stimulate success and those
that are negative i.e., reduce or completely halt the education
success. In addition, it was also emphasized that psychosocial
factors are more susceptible to control and that they can be much
more influenced compared to anatomic-physiologic ones [22]. Kresić
et al. [16], as well as Del Rio Valerias et al. [14] present a
division of factors into 3 groups i.e., patient-related,
treatment-related and rehabilitation-related ones. Next, Singer et
al. in their meta-analysis [23] label these factors as
socio-demographic, psychosocial and treatment-related ones, while
Frith et al. [20] group them as surgical, psychological, social and
physiological. In connection to that, in positive
anatomic-physiologic factors, according to Salmon [22], emphasized
is the significance of soundness and mobility of the
oropharyngoesophageal region i.e., function of lips, tongue and
velopharyngeal mechanism in order to provide a sufficient amount of
air and overcome the PE segment resistance, but also to achieve an
adequate relaxation of the same which is of utmost importance if the
inhalation method is used in rehabilitation. It is generally known
and mentioned that upon using the esophageal voice and speech the
esophagus acts as an air reservoir, and therefore, Salmon [22], but
also Singer et al. in their meta-analysis [23], point out that for
the success of its education, soundness of the function of all its
sphincters is needed in order to enable stopping i.e. proper flow of
the airstream. Stanković [7] also mentions the hearing status as a
significant positive factor which affects the education success,
since the adequate hearing function enables auditory control of
one’s own speech as well as the instructions relating to the
techniques and education while, on the other side, Singer et al.
[23] mention the lack of connection of this factor with the success
itself. According to Dragičević [4], patients with moderately severe
hearing impairment pronounce fewer number of syllables in one minute
and, in line with the previously mentioned studies, the same author
also mentions worse audio-vocal feedback in them. Salmon [22] points
out that the age is proved to be a success predictor i.e., that
younger individuals master the esophageal voice and speech with more
success because they are more motivated, determined, flexible.
Similarly, Singer et al.[23]mention this factor in their
meta-analysis as an important one i.e., pointing out that, the older
the patient is, the more pronounced the negative relatedness to
education success is. Such citations are confirmed by Frith et al.
[20] in their research. On the other hand, according to data from
the study of Del Rio Valeiras et al. [14], patients between age 51
and 60, mostly female population, showed greater success of the
esophageal voice and speech education but, however, gender- and
age-related factors did not prove to be significant success
predictors in this case. Same data relating to these factors were
also mentioned by Dragičević [4]. With regards to gender, in their
study, Keszte et al. [9] stated that in the female population there
is a higher level of stress and that the feeling of stigma is more
present because of the low frequency of the esophageal voice that is
60-70 Hz, which significantly differs compared to the frequency of
the healthy laryngeal female voice which can reach 220Hz [9].
Accordingly, Stanković [7] provides a detail that only 33.7% of
laryngectomized women accept the education of esophageal voice and
speech as a possible method and, according to the study conducted by
Frith et al [20], they spent much more time in rehabilitation,
rating it as extremely hard. In addition, Singer et al. [23] also
mention that the patients consider eructation inappropriate, and
therefore all mentioned factors may affect the success. It is also
important to point out the good general condition as a significant
factor that will definitely enable the success and contribute to it,
dictating actually the very beginning and the flow of the education
[22,23]. On the other hand, according to Salmon [22], negative
anatomic-physiologic factors are a combination of radiotherapy and
additional surgical treatments on bigger tumors because postsurgical
radiotherapy contributes to the dryness of mouth cavity, frequent
inflammations, discomfort when swallowing, which all reflect on the
very act of esophageal voice and speech education which is also the
case in swallowing disorders as such. Singer et al. [23] mention
swallowing disorders as negative predictors of unsuccessful
esophageal voice and speech education which reduce it significantly.
In their study, Del Rio Valeiras et al. [14] also present data
supporting the idea that the quality of the voice of patients who
received radiotherapy is worse compared to patients who did not,
while Cocuzza et al. [18] put forward that it improves with time
because the tissue itself is less flexible in early postradiotherapy
period and therefore it increases with time. Negative effect of
radiotherapy is recorded by Dragičević and Stanković[4,7]. According
to Singer et al.[23], radiotherapy as such does not affect the
success of the education. Furthermore, by introducing radiotherapy,
the vocal rehabilitation process is interrupted and so the
significant time period suitable for learning is lost. Salmon and
Stanković [22,7] point out that in cases of extended surgical
interventions, the structures that affect the esophageal speech
adoption itself, such as a part of pharynx, tongue or velum, are
removed as well. In this case, the education will be aggravated and
its success limited. Unlike Salmon’s [22], Del Ria Valerias et al.’s
[14] study provides an interesting detail that the radicalism of the
surgical resection does not significantly affect the success. The
same conclusion was reached by Dragičević [4] while, on the other
hand, Sokal et al. [24] suggest that the patients who underwent
radical surgical interventions have greater education success
compared to those who only underwent laryngectomy. Unfortunately,
what often happens, limiting the education, and even leading to its
regression, is the recurrence of the tumor, presence of metastases
and various complications. In that case, it is of primary importance
to remove the mentioned and stabilize the general condition of the
patient. In addition, according to Salmon [22], velopharyngeal
incompetence as well as velum paresis, may negatively affect the
esophageal voice and speech education by injection method. However,
in such case, it is possible to use the aspiration method, but it is
important to mention that the intelligibility of speech may be
impaired. What might negatively affect the air intake are definitely
the reduced tongue mobility and the presence of the anterior
pharyngeal diverticulum. These factors contribute to that fact that
the patient employs much more force than usual in order to achieve
the adequate pressure level and voice whose quality is similar to
one which requires less force. In their meta-analysis, Singer et al.
[23] also point out good tongue mobility as the factor that
positively correlates with the success. It is also important to
point out the effect of the presence of esophageal stenoses as well
as contraction of the inferior pharyngeal constrictor instead of
relaxation, hypertonicity of the PE segment, which further lead to
air retention in the hypopharynx but also its inadequate entry and
exit. All the mentioned affect the success of the esophageal voice
and speech education techniques [22]. The focus shifts to
psychosocial factors, where among the positive ones i.e., those that
accelerate the success of the esophageal voice and speech education,
Salmon [22] but also Singer et al. [23] mention readiness to
practice, which is more often long-lasting and intensive, presence
of motivation which has been mentioned in many papers by different
authors as the factor that affects the success of the education, and
also the acceptance of such voice, with all its characteristics,
which contributes to the increase of the level of its use in
communication, and also affects the patient’s self-confidence.
Interestingly, personality traits are mentioned in the Salmon’s [22]
study as an important factor, which leads to a situation that the
extroverts i.e., those who are more open for communication, have
contact with more people, achieve greater success in education
compared to introverts who possess opposite traits. Additionally,
the support of the family was mentioned as an important factor, but
also the importance of characteristics and features of the expert
who conducts the rehabilitation, which all together improves and
increases motivation that positively correlates with the education
success. The social activity itself, according to Singer et al.
[23], did not prove to be a significant factor that affects the
success of the esophageal voice and speech education, while, on the
other hand, personality traits of the patient are stated as
significant positive factors. Besides all positive factors, negative
ones are also very common, and mentioned meta-analysis as well as
the study of Del Rio Valeiras et al. [14] primarily put forward the
lack of motivation, presence of depression (which is often the
result of the radical surgery itself i.e. laryngectomy and loss of
the verbal communication function) and anxiety which impedes the
success itself that was also confirmed by Singer et al. [23] in
their meta-analysis. The lack of success may also be the result of
the patient’s inability to accept the current situation, lack of
support by the family and community, but also continued use of
alcohol and cigarettes, which are listed as main risk factors in
occurrence of malignant laryngeal tumors, may negatively affect the
education itself. However, the very use of alcoholic beverages,
according to papers comprised by Singer et al. [23] in their
meta-analysis, was mentioned as a factor with a lack of any
relatedness to success. Factors that are put forward as patient
related by Del Rio Valerias et el. [14] are his/her age and marital
status at the time of treatment, level of education, employment
before the intervention, current employment, place of residence,
where the focus is primarily on whether it is urban or rural
environment, and also the presence of some other diseases like
alcoholism, depression and others. In addition, these authors also
mention rehabilitation-related factors like the very technique used
in rehabilitation, the starting time, as well as the number of its
sessions. Singer et al. [23] found that the duration and frequency
of rehabilitation as such, do not significantly affect the very
success of the education. With regards to marital status at the time
of treatment and employment itself, according to Dragičević [4] and
Del Rio Valerias et al. [24] they are primarily related to the
motivation itself, self-confidence, amount of communication, quality
of social interactions the patient has, as well as the faster
adaptation to the current condition and situation. When we speak
about the education-related factor, according to Bunijevac et al.
[12], it does not affect the success of the education, which is also
confirmed by Singer et al. [23] and Dragičević [4], but he/she can
achieve it on the perception and evaluation of the quality of life
and therefore the patients with higher level of education rated the
quality of their lives as better in most cases [12]. According to
Del Rio Valerias et al. [14], the place of residence is related to
the remoteness of hospital centers where the treatment and
rehabilitation take place, and therefore the life in rural areas,
away from these centers, significantly complicates conducting and
success of esophageal voice and speech education. In addition,
Dragičević [4] mentions that the incidence rate of malignant
laryngeal tumors is higher in rural areas, and so we can draw a
parallel with the abovementioned. In their meta-analysis, Singer et
al. [23] singled out papers that mention even 24 factors that may
affect the success of the esophageal voice and speech education and
emphasized their positive and negative relatedness, non-compliance
and lack of relatedness with the success of education, and such
factors are primarily as follows: age, socio-economic status,
marital status, employment, support of the family and community,
personality traits, intellectual abilities and cognitive status,
motivation, psychosocial adaptability, communication behavior,
social activity, mental health, use of alcohol, length and quality
of rehabilitation, extended surgical interventions, stadium in which
malignant tumor was identified, its location, what type of
alaryngeal voice was used, patient’s hearing status, presence of
swallowing issues, tongue mobility, radiotherapy, postoperative
complications, general physical condition of the patient. Positive
relatedness to the success of the esophageal voice and speech
education was found when analyzing factors that are related to the
communication behavior, employment, tongue mobility, motivation,
psychosocial adaptability and personality traits. It is also
important to mention discordant results i.e., that in some studies
factors related to intellectual abilities, cognitive status,
socio-economic status and social support proved to be very
significant success predictors, while in others they were not
mentioned as significant ones [23]. When it comes to intellectual
abilities and cognitive status, according to Dragičević [4], there
is a positive correlation between this factor and perseverance in
rehabilitation i.e. more intelligent patients and those with better
cognitive status are more persistent in it, and this can also be
associated with the fact that the mentioned strive towards
establishing of the alaryngeal voice as soon as possible because in
most cases they are employed and in high positions that require
greater use of speech. On the other hand, according to Singer et al.
[23], negative relatedness to success occurs in factors related to
general physical condition of the patient, age, presence of
swallowing issues, occurrence of mental health problems (most often
depression), and also the occurrence of complications after the
surgery, while the lack of relatedness was noticed in factors like
use of alcohol, marital status, social activities, stadium and
location of the tumor, hearing status, education, duration and
quality of rehabilitation, extension of the surgery, radiotherapy.
In the research conducted by Kresić et al. [16], the impact of
motivation, gender, age, education and profession of the patient,
volume of the surgical resection, time of starting and duration of
the vocal rehabilitation, as well as the method used during the
course on the esophageal voice and speech education, were analyzed.
What is interesting is the fact that, according to this study,
motivation and duration of rehabilitation are considered as factors
that affect the education success, while in others such impact was
not manifested, which is in line with the previously mentioned
studies. In addition, mentioned is a detail that it is never too
late to begin with rehabilitation, which is by all means a
motivating piece of information for the patients, while Del Rio
Valeiras et al. [24] stated that is should be conducted as soon as
possible, emphasizing that it, as a factor, does not significantly
affect the success of the education itself. In addition, what also
stands out is the information that the duration will greatly depend
on the individual characteristics of the patient. In their study,
Frith et al. [20] came across results that are in line with the
results of Del Rio Valeiras et al. [24], whereby they emphasized
that the duration of rehabilitation and the time elapsed after the
surgical intervention do not affect the success. In their study,
Sokal et al. [24] point out that the patients whose rehabilitation
lasts longer, show greater success in esophageal voice and speech
education, which is in line with the research of Kresić et al. [16].
Some authors investigated if the way of conducting the esophageal
voice and speech education affects its success and in connection to
that, they compared individual and group work with patients.
According to Veselinović [25], individual approach has great
importance in the very beginning of the education because in that
period the patient is becoming familiar with and introduced to the
way the air is deposited in esophagus, act of eructation and
esophageal voice techniques as well as speech in general, but after
that, it would be useful for him/her to join the group in which
patients are similar, based on criteria like age, education, time
elapsed after the surgical intervention, intellectual and cognitive
status. In addition, this author points out that the approach i.e.,
factor related to group or individual education, does not have much
impact on its success while, on the other hand, Quing et al. [26] in
their research, came to the results that speak in favor of the fact
that group education significantly affects the success and this is
attributed to the increase in patient’s self-efficacy. Namely, when
this type of education is conducted, Quing et al. [26] mention that
patients develop the sense of belonging, because they meet people
who have an identical or at least similar problem like they do,
which leads to significant increase in self-confidence and
motivation, and decrease of negative emotions and other factors that
limit them. In addition, there is an exchange of experience both
between the patients and between their families, which is a very
important factor in the overall rehabilitation process. Another
factor that is being mentioned as one of those that may affect the
success of the esophageal voice and speech education is the presence
of the gastroesophageal reflux. In his study, Mathis [27], mentions
that the lower esophageal sphincter competence disables adequate air
retention, which is also contributed by the leak backward of the
stomach content, and resulting in acid causing contractions of the
upper esophageal sphincter, and even its spasm. The research showed
that the gastroesophageal reflux does not affect the success of the
esophageal voice and speech education i.e., that the skilled, less
skilled or completely unskilled users of the esophageal voice and
speech had the same incidence of the gastroesophageal reflux after
all trials, which was also confirmed by Dragičević [4] in her PhD
thesis. What stands out as important is the fact that the esophageal
reflux as such occurs more often in patients who use esophageal
speech in order to communicate, which brings it into connection with
the eructation itself [27].
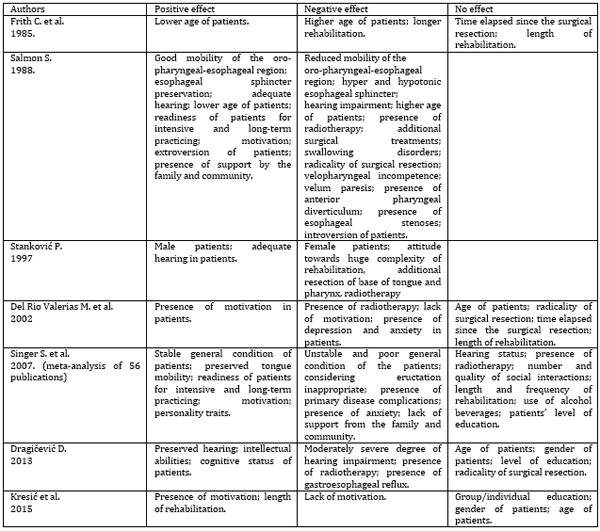
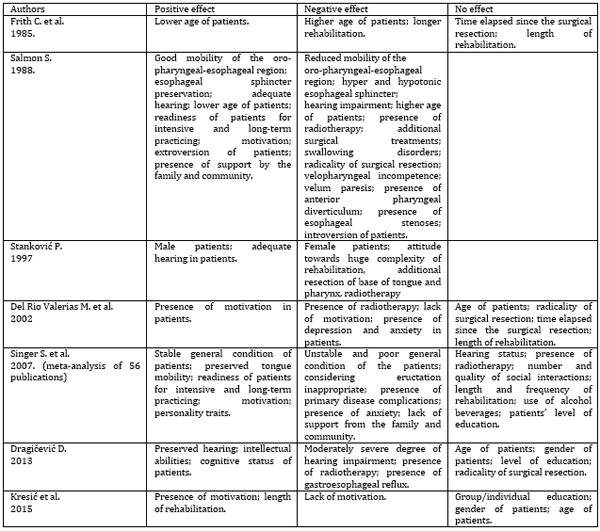
The most significant factors affecting the success in mastering the
esophageal voice and speech are shown in table 1.
Table 1: Presentation of factors that affect the
success of the esophageal voice and speech education
4. DISCUSSION
The questionable issue and the reason why we come across
different data about success, but also about factors that impact
them, is dissimilarity i.e., lack of uniform criteria for its
evaluation. Authors of research and meta-analyses comprised with
this review used different criteria for evaluation of success,
depending on their country of origin and those they considered most
suitable for the evaluation itself. Different criteria also resulted
in different interpretation of the factors which positively i.e.,
negatively affect the success.
Criteria that have most often been mentioned in literature relate to
satisfactory phonation when needed, length of air insufflation,
short latency between inhalation and beginning of phonation, good
intelligibility [4,28]. When it comes to overall impression,
Stanković [7] provides a five-level scale, which evaluates the
quality of esophageal voice i.e. evaluates the parameters related to
the quality, roughness, clarity, weakness of the voice and vocal
strain, and the levels are as follows: 1. excellent – full
automatism in speech production; 2. good – continuous speech with
occasional soundlessness of certain syllables; 3. mediocre – the
technique is present, but without longer continuity; 4. Poor-
production of short phrases only and 5.very poor/failed - production
of only certain two-syllable and multi-syllable words or no sound at
all. The same scale was also used by Mumović et al. [28] as well
Vekić et al. [29].
According to Kresić et al. [16], excellent success in esophageal
voice and speech education was achieved by patients who have fully
automatized it, while the success rated as good implies establishing
continuous speech with soundlessness of certain syllables, which
matches Stanković’ [7] criteria. Somewhat more elaborately defined
criteria are found in Veselinović et al.’s [13] paper, where the
success is rated as excellent in cases when a patient has the
ability to spontaneously and effortlessly produce esophageal voice
and speech in every communication situation, which is fully
automatized and with a steady rhythm and melody, barely noticeable,
deprived of the noise of cannula, and without too much unnecessary
gesturing. On the other hand, one finds a definition arising from
the fact that the education is considered successful if the patient
has the ability to communicate with his/her environment in any way,
and that such communication is also socially acceptable. In
addition, the criterion of success is, on one hand, also rated based
on whether the patient uses the learnt voice and speech at all, what
their qualities are, whether he/she uses such way of communication
as the only one while, on the other, it is rated by estimating
phonation parameters like intelligibility, pitch, loudness, speed,
but also the satisfaction of the patient with his/her own voice and
speech [4]. Criteria for assessment of success used by Del
RioValeiras et al. [14] imply three levels i.e., good success of the
esophageal voice and speech education is achieved when a person
always uses it, it is medium if the person uses it sometimes and
poor if he/she does not use it at all.
From the above said, we can realize that by watching the criterion
which implies that the patient spontaneously and effortlessly
produces esophageal voice and speech in every communication
situation, in a fully automatized way and with a steady rhythm and
melody, barely noticeable, deprived of the noise of cannula, and
without too much unnecessary gesturing, the success can be
characterized as significantly smaller compared to one whose
criterion is that the patient can communicate in any way that is
socially acceptable, and therefore the factors that affect it will
be observed differently [4,13].
Besides the lack of consistent criteria, the reasons for divergence
of results and different recording of the impact of individual
factors on the success itself are also the use of different
measuring instruments, which are often not standardized i.e., rules
for their use, scoring and interpretation of data are not defined
beforehand [23]. It is preferable to use the objective analysis
which reduces the probability that it will produce its own
conclusion, different processing and interpretation, which will
definitely affect the improvement of success evaluation, but the
perception of the factors’ impact as well. However, its drawback is
that it requires the use of voice sample only, but not speech
[4,23]. When speaking about the instruments for self-assessment by
the patients, a problem arises, implying different perception of the
quality of voice and speech, and therefore the success of the
education. For that reason, the esophageal voice and speech that was
rated as excellent according to a therapist’s evaluation, the
patient shall consider unsatisfactory because he/she makes the
comparison against the former, premorbid characteristics, while, on
the other hand, voice and speech that were rated as very poor by a
therapist, could be very satisfactory and excellent to the patient
because for him/her the quality is not of primary importance. In
connection to that, according to Dragičević et al. [30], patients
who use esophageal voice and speech as a method of alaryngeal
communication, rated its quality significantly worse compared to
those who use tracheoesophageal voice and speech. In addition,
disagreement with regards to the impact of factors on the success of
education also results from inclusion of small number of examinees
in the studies, and therefore the results cannot be largely
generalized with regards to the entire population of laryngectomized
patients who were educated for the use of esophageal voice and
speech. What has been put forward as significant is also the need
for a multi-variant analysis in order to perceive the manifestation
and realization of the impact of factors on one another [23].
5. CONCLUSION
When taking into account all effects of the total laryngectomy
and loss of numerous laryngeal functions on a person, among which is
the most important one for them – phonation function, esophageal
voice and speech education represents the most natural and humane
type of reestablishment of verbal communication, despite the fact
that in developed countries it has been completely replaced by the
primary implantation of vocal prosthesis, especially in last 30
years. As pointed out, there are still not clearly defined,
generally accepted and comprehensive criteria to evaluate to what
extent the esophageal voice and speech education was successful, and
this results in different understanding of the same, and then
different understanding of positive i.e., negative impact of
different factors. Despite the abovementioned, most of the conducted
studies examining the factors that may affect the success of the
esophageal voice and speech education, speak in favor of the fact
that the patient’s motivation is the key to the same. In all other
factors, different data were obtained, and in some cases, they do
affect the success, but in some, their impact is completely absent.
What needs to be done in the future is to clearly define the success
criteria, but also define and apply standardized instruments in
order to enable more adequate examination of the success of the
esophageal voice and speech education, and compare the results of
different studies. In addition, an evaluation with objective
assessments of various voice and speech parameters on representative
sample of participants is required.
6. LITERATURE:
- Bunijevac M, Petrović Lazić M, Jovanović Simić N, Maksimović
S. Uticaj radioterapije na kvalitet života laringektomisanih
pacijenata pre i posle vokalne rehabilitacije. Medicinski
Timočki glasnik. 2018;43(2):41-8.
- Bunijevac M, Petrović Lazić M. Značaj rane vokalne
rehabilitacije i kvalitet života laringektomisanih pacijenata.
Specijalna edukacija i rehabilitacija. 2016;15(4):379-93.
- Dragičević D, Anđelić B, Jović MR, Kljajić V, Vlaški Lj,
Savović S. Clinical stage of laryngeal carcinoma and lost time
at the moment of diagnosis with 15-year-long interval. Are there
any changes? J BUON. 2019;24(5):2041-8.
- Dragičević D. Govorna rehabilitacija totalno
laringektomisanih pacijenata ugradnjom vokalnih proteza
[doktorska disertacija]. Novi Sad: Univerzitet u Novom Sadu,
Medicinski fakultet; 2013.
- Šehović I, Petrović Lazić M, Jovanović Simić N. Akustička i
perceptivna analiza ezofagealnog i traheoezofagealnog glasa.
Specijalna edukacija i rehabilitacija. 2017;16(3):289-307.
- Mumović G. Konzervativni tretman disfonija. Novi Sad:
Medicinski fakultet; 2004.
- Stanković P. Fonijatrijska rehabilitacija laringektomisanih
pacijenata uspostavljanjem ezofagusnog glasa i govora
modifikovanom Semanovom metodom [doktorska disertacija].
Beograd: Univerzitet u Beogradu, Medicinski fakultet; 1997.
- Milovanović J, Jotić A, Tešić Vidović Lj, Đukić V, Trivić A,
Krejović Trivić S et al. Survival outcomes in surgically treated
patiens with advanced laryngeal cancer in Serbia. Vojnosanit
pregl. 2020;77(9):885-92.
- Keszte J, Wollbrück D, Meyer A, Fuchs M, Meister E, Pabst F
et al. The Role of Sex in Voice Restoration and Emotional
Functioning After Laryngectomy. Laryngo-Rhino-Otol.
2012;91:240-6.
- Jović MR, Mumović MG, Mitrović MS, Golubović S. Medicinske
osnove poremećaja glasa i govora. Novi Sad. Medicinski fakultet;
2014.
- Krishnamurthy A, Khwajamohiuddin S. Analysis of Factors
Affecting the Longevity of Voice Prosthesis Following Total
Laryngectomy with a Review of Literature. Indian J Surg Oncol.
2018;9(1):39-45.
- Bunijevac M, Petrović Lazić M, Maksimović S. Uticaj
obrazovanja na kvalitet života laringektomisanih bolesnika pre i
posle vokalne rehabilitacije. Biomedicinska istraživanja.
2019;10(1):30-7.
- Veselinović M, Jovanović Simić N, Arbutina T, Petrović Lazić
M, Škrbić R. Karakteristike traheoezofagusnog glasa i govora
laringektomisanih pacijenata posle primarne i sekundarne
ugradnje vokalne proteze. Specijalna edukacija i rehabilitacija.
2012;11(2):247-63.
- Del Rio Valerias R, Martin Martin C, Perez-Carro Rios A,
Minguez Beltran I, Rodriguez Martul C, Bravo Juega E et al.
Estudio de posibles factores que inflyen en la rehabilitacion
laringuectomizado total mediante voz ezofagica. Acta
Otorinolaringol Esp. 2002;53:413-17.
- Shuxin X. Effectiveness of voice rehabilitation on
vocalisation in postlaryngectomy patients: a systematic review.
Int J Evid Based Healthc. 2010;8:256-58.
- Kresić S, Veselinović M, Mumović G, Mitrović MS. Possible
factors of success in teaching esophageal speech. Med Pregl.
2015;68(1-2):5-9.
- Doyle CP, Finchem AE. Teaching Esophageal Speech: A Process
of Collaborative Instruction. Clinical Care and Rehabilitation
in Head and Neck Cancer. 2019;145-61.
- Cocuzza S, Maniaci A, Grillo C, Ferlito S, Spinato G, Coco S
et al. Voice-Related Quality in Life in Post-Laryngectomy
Rehabilitation: Tracheoesophageal Fistula’s Wellnes. Int J
Environ Res Public Health. 2020;70(10):407-23.
- Krejović Trivić S, Milovanović J, Parapid B, Vukašinović M,
Miković N, Trivić A. Quality of life of laryngectomized patients
in Serbia. Srp Arh Celok Lek. 2018;146(11-12):657-62.
- Frith C, Buffalo DM, Montague CJ. Relationship between
esophageal speech proficiency surgical biographical, and social
factors. J Commun Disord. 1985;18:475-83.
- Gates AJ. Predicting esophageal speech. Ann Otol Rhinol
Laryngol. 1982; 91:454-7.
- Salmon JS. Factors predictive of success or failure in
acquistion of esophageal speech. Head Neck Surg. 1988;10:105-9.
- Singer S, Merbach M, Dietz A, Schwarz R. Psychosocial
Determinants of Successful Voice Rehabilitation After
Laryngectomy. J Chin Med Assoc. 2007;70(10):407-23.
- Sokal W, Kordylewska M, Golusinski W. An influence of some
factors on the logopedic rehabilitation of patients after total
laryngectomy. Otolaryngol Pol. 2011;65(1):20-5.
- Veselinović M. Individualni i grupni tretman u edukaciji
ezofagusnog govora laringektomisanih pacijenata. [Završni rad na
diplomskim akademskim studijama]. Novi Sad: Univerzitet u Novom
Sadu, Medicinski fakultet; 2011.
- Quing C, Jing L. Jun-ping L, Dan-ni J, Yong Y, Hong-xia R et
al. Influence of Collective Esophageal Speech Training on
Self-efficacy in Chinese Laryngectomees: A Pretest-posttest
Group Study. Curr Med Sci. 2019;39(5):810-15.
- Mathis GJ, Lehman AG, Shanks CJ, Blom DE, Brunelle LR.
Effect of Gastroesophageal Reflux on Esophageal Speech. J Clin
Gastroenterol. 1983;5:503-7.
- Mumović MG, Mitrović MS, Jović MR. Praktikum iz medicinskih
osnova poremećaja glasa i govora. Novi Sad. Medicinski fakultet;
2014.
- Vekić M, Veselinović M, Mumović G, Mitrović MS. Articulation
of sounds in serbian language in patients who learned esophageal
speech successfully. Med Pregl. 2014;67(9-10):323-7.
- Dragičević D, Jović RM, Kljajić V, Vlaški Lj, Savović S.
Comparison of Voice Handicap Index in Patients with Esophageal
and Tracheoesophageal Speech after Total Laryngectomy. Folia
Phoniatr Logop. 2020;72:363-9.
|
|
|
|