|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
Page 126 |
||||||||||||||||||||||||||||||||||||
|
Case report The significance of oral anticoagulant therapy in the prevention of thromboembolic complications in patients with atrial fibrillation during a 14-year follow-up - Case report Anastasija Raščanin (1), Dušan Bastać (1), Mila Bastać (2) (1)OFFICE OF INTERNAL MEDICINE "DR BASTAĆ", KOSANČIĆEV VENAC NO. 16, ZAJEČAR; (2) MEDSCAN TADIĆ DIAGNOSIS, ZAJEČAR |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | INTRODUCTION. Atrial
fibrillation (AF) is the most common long-term arrhythmia and
represents one of the main public health problems primarily due to
the aging of the general population, in which this arrhythmia occurs
more often and causes thromboembolic stroke. Cardioembolic stroke
associated with AF is usually severe, highly recurrent, and often
fatal or with permanent disability of specific stroke risk
factors/modifiers. Common risk factors are summarized in a risk
factor-based clinical score called the CHA2DS2-VASc Score. Poor INR
control increases the risk of both thromboembolic and hemorrhagic
complications, and the optimal balance between the benefits and
risks of using oral VKAs is achieved when the TTR, or time in the
therapeutic range, is ≥ 70% [9]. We present the case of a female
patient that confirms the importance of oral anticoagulant therapy
when the INR is in the therapeutic range between 2-3, in the largest
number of measurements in the successful prevention of recurrent
thromboembolic complications during a 14-year follow-up. CASE
REPORT: We present a 60-year-old MD patient who first came to the
Office of Internal Medicine "Dr. Bastać" in 2008 due to a feeling of
instability and heart palpitations. Due to grade II hypertension,
which is not well regulated, she has been taking antihypertensive
therapy for the past two years, treats elevated cholesterol with
statins, and states that in two years and a year before her first
examination at the Office of Internal Medicine "Dr. Bastać", she had
two minor strokes verified by MSCT of the endocranium. In our
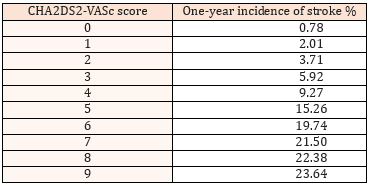
patient, a high CHA2DS2-VASc score of 4 was calculated
(hypertension, female gender and previous stroke) and the estimated
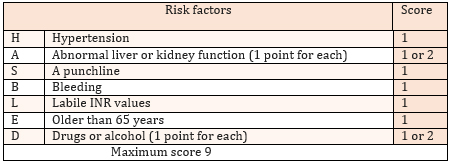
annual risk for stroke is 9.27% (TABLE 2). Her bleeding risk - HAS
BLED Score is moderate and is 2 (hypertension, CVI). Based on
CHA2DS2-VASc, the risk of adverse thromboembolic events is high and
requires the introduction of oral anticoagulant therapy. The patient
in therapy receives acenocoumarol according to the scheme so that
the value of PT/INR is between 2.0 and 3.0. Good anticoagulation is
defined as having 3 to 4 PT/INR values in the therapeutic range
(similar to TTR 50 to 60% of the time), while poor anticoagulation
is: 0-2 measured INR values in the therapeutic range (TTR <50%) [3].
In our patient, the TTR is about 70%, which represents excellent
anticoagulation. During 14 years of monitoring for three months, as
well as at the recent control on 04/29/2022. the patient feels well,
with no new thromboembolic complications and no bleeding episodes.
CONCLUSION. Antithrombotic therapy with vitamin K antagonists can
achieve good anticoagulation and long-term successful prevention of
repeated cardioembolic strokes in patients with atrial fibrillation.
We emphasize the need for highly motivated patients to regularly
monitor the level of anticoagulation via INR and the full engagement
of the prescribing physician. In this case, we emphasize the
frequent problem of delays in the introduction of anticoagulation
therapy in atrial fibrillation. Stroke prevention is the cornerstone
of care for patients with atrial fibrillation. Key words: atrial fibrillation, stroke prevention, thromboembolic stroke, vitamin K antagonists, non-vitamin K anticoagulant drugs, INR, TTR |
|||||||||||||||||||||||||||||||||||
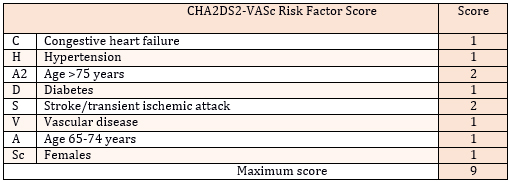
INTRODUCTIONAF is the most common long-term arrhythmia and represents a major public health problem. It is estimated that the number of patients will progressively increase in the next few decades, primarily due to the aging of the general population, in which this arrhythmia occurs more often [1]. Atrial fibrillation (AF) is characterized by disorganized, rapid, and irregular activation of the atria, with a lack of atrial contraction and irregular ventricular rate. Absolutely irregular RR intervals (which is why it is also called absolute arrhythmia), lack of P waves, and atrial frequency higher than 300/min, are registered electrocardiographically. Risk factors for developing AF, in addition to age, include hypertension, diabetes mellitus, heart disease, and sleep apnea. AF increases the risk of ischemic stroke fivefold. Cardioembolic stroke associated with AF is usually severe, highly recurrent, and often fatal or with permanent disability [2]. Ischemic stroke in patients with AF is most often caused by the dissemination of a thrombus formed in the auricle of the left atrium [3]. The risk for stroke associated with AF is not homogeneous, considering that it depends on the presence of specific stroke risk factors/modifiers. Common risk factors are summarized in a risk factor-based clinical score called the CHA2DS2-VASc Score, in which congestive heart failure, hypertension, age 65-74 years, diabetes, peripheral vascular disease, and female gender contribute 1 point each, while previous ischemic stroke or transient ischemic attack (TIA) as well as age ≥ 75 years carry 2 points (TABLE 1). Lifelong anticoagulant therapy is always recommended in patients with atrial fibrillation for stroke prevention when the CHA2DS2-VASc score is > 2 in men and > 3 in women (recommendation class I, level of evidence A), and may be considered in CHA2DS2-VASc score = 1 in men or = 2 in women (recommendation class IIa, level of evidence B) [ 4 ]. TABLE 1 CHA2DS2-VASc Score: Clinical Risk Factors for Stroke, Transient Ischemic Attack
TABLE 2 One-year frequency of stroke (%) in AF according to CHA2DS2-VASc score
Before initiating oral anticoagulant therapy, the risk of bleeding should be assessed using the HAS-BLED score (hypertension, abnormal kidney/renal function, stroke, bleeding history or predisposition, labile INR, age over 65 years, drug/alcohol use) and if it is high, i.e. over 3, the correction of modifiable risk factors should be considered and those patients should be monitored more often, but certainly a high score is not a reason to stop anticoagulant therapy (recommendation class IIa, level of evidence B ) (TABLE 3) [5 ]. TABLE 3. HAS-BLED Score: assessment of bleeding risk for patients with AF
For more than 60 years, vitamin K antagonists (VKA) have been
used to prevent stroke in patients with AF [6]. Oral VKAs are
coumarin derivatives that inhibit the synthesis of vitamin
K-dependent coagulation factors (II, VII, IX and X) in the liver.
Representatives of this group of drugs are acenocoumarol, warfarin,
and rarely phenprocoumon [7]. The safe and effective use of these
drugs implies regular control of indicators of the intensity of the
anticoagulant effect of vitamin K antagonists, the INR
(international normalized ratio of prothrombin times), which should
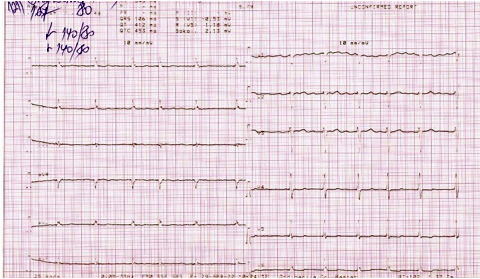
be in the range of 2.0 to 3.0 [ 8 ] . Material and methodsThe material used for the preparation of this paper was the patient's electronic health record as well as his personal medical documentation (laboratory analysis findings, specialist doctor's reports and discharge list). The method of retrospective analysis of medical records was applied. Case presentationThe case is about a 60-year-old MD patient who came to the Office of Internal Medicine "Dr. Bastać" for the first time in 2008 due to a feeling of instability and heart palpitations. Due to grade II hypertension, which is not well regulated, she has been taking antihypertensive therapy for the past two years, treating elevated cholesterol with a statin. She has had palpitations and arrhythmia for the last 2 years, two years ago and a year before her first examination at the Office of Internal Medicine"Dr. Bastać" office, she had two minor strokes verified by MSCT of the endocranium. The patient is a non-smoker, pre-obese BMI 29.0 with pronounced abdominal obesity (waist circumference 104 cm). During the physical examination, we determined that the patient was cardiopulmonarily compensated and hemodynamically stable. Heart rhythm was irregular, tones were clear, murmurs were not registered. Blood pressure on arrival, measured brachially bilaterally, was 170/100 mmHg. Auscultation of the lungs revealed a normal respiratory murmur. The liver was not enlarged and there was no pretibial edema. Hematological and biochemical analyzes were within normal limits. ECG on arrival: atrial fibrillation, fr 85/min, normogram, incomplete left bundle branch block, horizontal depression ST -0.5 in V5-V6 (Figure 1). Figure 1. ECG on arrival from 2008
Echocardiographic findings from 2008 indicate that the left
ventricle was of normal dimensions without myocardial hypertrophy
and with preserved global systolic function. There were no segmental
outbursts in the contractility of the left ventricular walls. Mitral
cusps were slightly more voluminous with minor mitral regurgitation.
Left sternum dilated, 39 mm measured in a standard parasternal
section. Right ventricle of normal dimensions. DISCUSSIONIn the last few years, several phase III randomized clinical
trials comparing the effect of new oral anticoagulant drugs with
warfarin in the prevention of thromboembolism in AF have been
completed. The new drugs are divided into two groups: oral direct
thrombin inhibitors (dabigatran) and oral direct factor Xa
inhibitors (rivaroxaban and apixaban). The advantage of the new
drugs lies in the smaller number of clinically significant
interactions with food and other drugs and the absence of the need
for regular laboratory monitoring of the anticoagulant effect, with
equal effectiveness in the prevention of thromboembolism and a lower
frequency of significant bleeding compared to VKA (10,11). But the
presented case shows that long-term successful prevention of
repeated cardioembolic strokes in patients with permanent atrial
fibrillation can also be achieved with classic antithrombotic
therapy with VK antagonists. CONCLUSIONThe presented case confirms the view that, even in the era of new
anticoagulant drugs NON-VK antagonists (NOACs), classic
antithrombotic therapy with Vitamin K antagonists can achieve good
anticoagulation and long-term successful prevention of repeated
cardioembolic strokes in patients with permanent as well as
paroxysmal atrial fibrillation based on CHA2DS2-VASc score without
significant hemorrhagic complications, the risk of which we assess
HAS BLED Score REFERENCE:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||