|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
Page 5 |
||||||||||||||||||||||||||||||||||||
|
Original paper Self-assessment of pharmacists regarding the practice of dispensing antibiotics in public pharmacies Slađana Ž. Zivanovic MELISA PHARMACY, MAJUR, ŠABAC, SERBIA |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Download in pdf format | Summary:
Introduction: Approximately at the end of one century after the
discovery of penicillin, the world is facing the development of
bacterial resistance to antibiotics. The focus of our work is the
pharmacist, as one of the key actors in the chain of antibiotic
dispensing. Through research, we aimed to determine the level of
knowledge among employees in pharmacies in the city and municipality
of Šabac in the Republic of Serbia about antibiotics, antimicrobial
resistance, the legal framework regulating the area of antibiotic
dispensing, as important factors for self-assessment in the practice
of antibiotic dispensing in public pharmacies. Objectives: (1) to
examine the knowledge of pharmacy employees about antibiotics,
antimicrobial resistance (AMR), and the legal framework regulating
the area of antibiotic dispensing; (2) to investigate the practice
of antibiotic dispensing in public pharmacies; (3) to assess
differences in the practice of antibiotic dispensing based on gender
of the respondents, pharmacy location, and level of education.
Methodology: A cross-sectional study was conducted using a
purposefully created questionnaire consisting of 33 questions,
through which respondents self-assessed their knowledge related to
antibiotics and the practice of antibiotic dispensing in the last
six months. Health workers of all levels of pharmacy education
employed in almost all pharmacies in the territory of the city of
Šabac (including city and rural pharmacies) participated in the
study. Data were collected from March to August 2022. Results: The
total number of respondents in the study was 229, with the majority
being female. Regarding formal education, the majority of
respondents were graduate pharmacists (59%), followed by higher
pharmacy technicians (3.5%) and pharmacy technicians (37.6%). When
it comes to viral infections, 95.2% of respondents knew that
antibiotics are ineffective in such cases; while 72.6% of
respondents believe that acute sore throat should not be treated
with antibiotics. As much as 99.6% of respondents confirmed the
statement that inappropriate use of antibiotics contributes to the
increase in antibiotic resistance. Also, 96.5% of respondents
confirmed that dispensing antibiotics without a prescription leads
to the development of antibiotic resistance. A total of 90.8% of
respondents are aware that pharmacists can be penalized in
accordance with existing legal regulations if they dispense
antibiotics without a prescription. In practice, dispensing
antibiotics without a prescription is still present in certain
situations. Although this phenomenon is not common based on survey
responses ("I always prescribe without a prescription at the
patient's request") for the surveyed locations of infections, it
occurs in a small number of cases, from 1.4% to 4.0%. However, based
on the response "I sometimes prescribe without a prescription at the
patient's request," it occurs more frequently in certain clinical
conditions and complaints: most commonly urinary tract infections in
52% of cases, infected wounds - 42.4%, acute sore throats in 29.8%,
and diarrhea - 15.7%, and least commonly for common colds and coughs
in 9.2%. At the patient's request, the majority of respondents -
79.9% never dispense antibiotics without a prescription, but still
globally 20.1% of respondents sometimes dispense antibiotics without
a prescription or doctor's report. Conclusion: Based on the results
of the sample of 229 pharmacist and pharmacy technician respondents,
it is concluded that dispensing antibiotics without a prescription
is still present in practice in certain situations. Although this
phenomenon is not common from responses: "I always prescribe without
a prescription at the patient's request" for surveyed locations of
infections (1.4% to 4.0%), and sometimes for certain conditions and
complaints, most commonly for common colds and coughs at 9.2% and
most commonly for urinary tract infections - 52%, At the patient's
request, 79.9% of respondents never dispense antibiotics without a
prescription, but still globally 20.1% of respondents sometimes
dispense antibiotics without a prescription or doctor's report.
Antimicrobial resistance is a systemic issue that undoubtedly
requires teamwork of all stakeholders in society where the role of
pharmacists and pharmacy technicians is one of the most significant. Keywords: antibiotics, antibiotic resistance, pharmacists, antibiotic dispensing in public pharmacies. |
|||||||||||||||||||||||||||||||||||
|
INTRODUCTION Antibiotics are becoming increasingly ineffective as drug
resistance spreads globally, leading to more severe infections and
increased mortality. Considering that several decades have passed
since the beginning of mass antibiotic use, the development of
bacterial resistance to antibiotics is an expected process of
evolution in terms of bacterial genetic adaptations to environmental
conditions. With the understanding that the number of bacteria
doubles every 20 minutes, it becomes clear how significant the
possibilities for resistance development are. Bacterial resistance
to antibiotics today poses one of the greatest threats to global
health [1]. While resistance to antibiotics occurs naturally,
irrational antibiotic use accelerates this process, resulting in
increased mortality, prolonged hospital stays, and higher medical
costs. According to antibiotic consumption data, the Republic of
Serbia ranks high among European countries, while a high level of
resistance is observed in all tested bacterial species in our
country, similar to countries in Southern and Eastern Europe [2].
Mass antibiotic use has led to a significant problem of
antimicrobial resistance (AMR) over time. AMR was initially
addressed by the development of new classes of antimicrobial agents
and chemical modification of existing ones. However, the development
of new antimicrobial drugs has not kept pace with the ability of
microbes to develop resistance. As a result, AMR is now a global
public health challenge and an escalating threat to infectious
disease control worldwide. AMR results in prolonged illness,
increased risk of infection spread, increased morbidity, and higher
mortality rates, with associated increases in financial and societal
costs [3]. OBJECTIVES The specialist work from which this text originated set three specific objectives that the conducted research needed to address:
As a general goal, the work aimed to empirically present the self-assessment of pharmacists regarding the practice of dispensing antibiotics in public pharmacies. THE METHODOLOGY The study was conducted as a cross-sectional study using a
purpose-designed questionnaire through which respondents
self-assessed their knowledge related to antibiotics and their
practices in dispensing antibiotics over the past six months. The
research involved healthcare workers of all levels of pharmacy
education (pharmacists, pharmacy masters, graduates, technicians)
employed in almost all pharmacies in the city of Šabac (including
both urban and rural pharmacies). Additionally, participants
attending the XV Professional Conference "Marketing in Pharmacy,"
held in Šabac on March 19, 2022, under the theme "New Knowledge,
Skills, and Competencies of Healthcare Workers - Challenges in the
21st Century," organized by the Pharmacy Institution "Melissa" and
the drugstore "Lin" from Šabac, were also included in the study.
Data were collected from March to August 2022. RESULTS During the research, a total of 400 questionnaires were
distributed to respondents. As the completion of the questionnaires
was based on a voluntary principle, out of the total number of
distributed questionnaires, 258 were completed, with 29 not fully
filled out. Therefore, the total number of respondents who completed
the questionnaire in a qualitatively satisfactory manner for use in
the research was 229, or 88.76% of the total number of completed
questionnaires. Looking at the gender structure of the
questionnaires used in the study, 200 respondents were female
(87.3%). In terms of formal education, the majority of respondents
were individuals with a completed pharmacy faculty degree –
pharmacists (59%), followed by higher pharmacy technicians (3.5%)
and pharmacy technicians (37.6%). The research showed that the
minimum number of pharmacists per pharmacy was one, while the
maximum was six. More than half of the pharmacies had two employed
graduated pharmacists (57%). Almost all pharmacists in pharmacies
had a license to practice (98.6%), with only 3 respondents
indicating that not all pharmacists in their pharmacies were
licensed. The average age of the respondents was 40.1 years, and the
average years of work experience were 14.4 years. Most respondents
worked in city pharmacies (47.6%), followed by pharmacies in smaller
towns (39.2%), while the smallest number worked in rural pharmacies
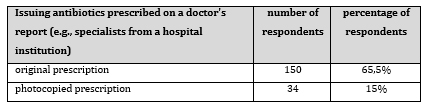
(13.2%). Table 1 - Distribution of responses regarding whether prescriptions from doctors should be original or photocopied
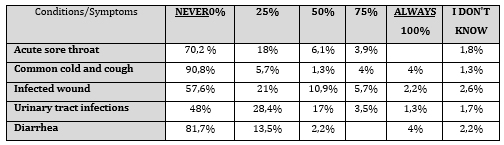
Responses to the question of whether antibiotics were dispensed without a prescription for specific conditions in the past month are presented in Table 2. Although this occurrence is rare based on the response "I always (100%) prescribe without a prescription at the patient's request," for the examined infection localizations, it was rare for the urinary tract - ranging from 1.3% to 4.0% for common cold and cough or diarrhea. However, based on survey responses: "I sometimes dispense antibiotics without a prescription (in a range of 25-75% of cases) for certain conditions i.e. infection localizations, this happens (most often in urinary tract infections - 52.0%, infected wounds - 42.4%, acute throat inflammation 29.8%, and diarrhea - 15.7%, and least often in common cold and cough - 9.2%. Despite the fact that the highest number - 79.9% of respondents never dispense antibiotics without a prescription at the patient's request, still 20.1% of respondents sometimes dispense antibiotics without a prescription or doctor's report. Table 2 - Distribution of responses to questions about whether respondents dispensed antibiotics without a prescription during the past month for the specified conditions, symptoms, or localization of potential
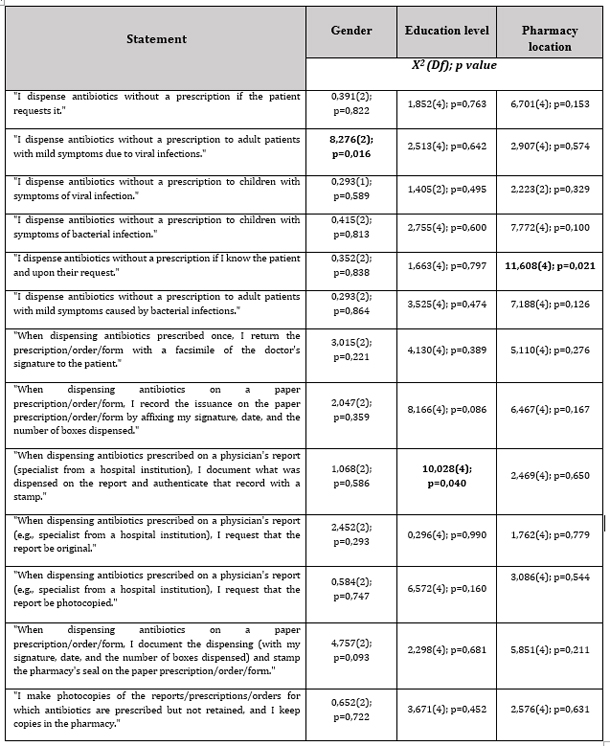
Results regarding the practice of antibiotic dispensing
concerning participants' gender, pharmacy location, and educational
level Table 3 - Responses regarding gender, educational level, and pharmacy location
The results we obtained show that in terms of gender, there is a statistically significant difference in responses only for the statement "I issue antibiotics without prescription to adult patients with mild symptoms due to viral infections." 6.9% of male respondents answered "sometimes," while only 0.5% of female respondents did so. A statistically significant difference in education level is observed for the statement "When issuing antibiotics prescribed by a hospital specialist, I document what was issued on the report and stamp that record with a seal." The response "always" was given by the majority of pharmacists (83.7%), followed by higher pharmacy technicians (75%), and then pharmacy technicians (68.6%). Although only licensed pharmacists are legally allowed to dispense prescription drugs, it is evident in practice that pharmacy technicians also dispense drugs because a high percentage of them responded positively to this question. Every pharmacy must have a responsible pharmacist present, and only in their presence can a pharmacy technician dispense medication. Personal connections with patients, the so-called "patient-oriented care" concerning the location of the pharmacy, is represented by the statement "I issue antibiotics without prescription if I know the patient, upon their request," and it is the only one that statistically differs in responses. Employees in pharmacies in smaller locations predominantly responded with "never" (79.8%). DISCUSSION If this study from Sri Lanka from 2016/17 is compared with our
research from 2022, several important observations can be made.
Firstly, the study from Sri Lanka had a national character,
considering that the survey was conducted across all provinces of
the country, while our research focused on one (micro)region (the
city of Šabac and its surroundings). Furthermore, antibiotics are
still dispensed without a prescription in both countries, despite
legislative frameworks prohibiting it; the knowledge of pharmacy
staff on the topic of antibiotics, AMR, and antibiotic dispensing
practices is significantly better in the Republic of Serbia;
knowledge about antibiotics is one of the reasons that significantly
influences the reduction of antibiotic dispensing without a
prescription, therefore, further education and raising awareness
about these issues in both countries are recommended; the level of
formal education of employees in the Republic of Serbia is higher
than that of their colleagues in Sri Lanka; personal acquaintance
with patients in both countries is a major reason for dispensing
antibiotics without a prescription; the profit motive is extremely
significant in both countries. Finally, awareness of AMR and its
harmful impact on the entire population cannot be left as a problem
only for pharmacy employees and patients. The significance of this
issue is such that it requires the activation of the entire society,
from the governments of all countries (including Sri Lanka and the
Republic of Serbia), which will incorporate this topic into public
health policies, to a broad action by media professionals to spread
awareness about these issues, revising educational programs,
improving educational plans for personnel being trained for
pharmaceutical activities, and other measures. CONCLUSION Self-assessment of pharmacists regarding the practice of
dispensing antibiotics in public pharmacies in the city and
municipality of Šabac in the Republic of Serbia was examined through
responses to 33 self-assessment questions from the completed
questionnaire. The results of the study show that regarding viral
infections, 95.2% of respondents know that antibiotics are
ineffective in such cases; 98.7% of respondents are confident that
common colds and coughs should not be treated with antibiotics,
while 72.6% of respondents believe that acute throat pain should not
be treated with antibiotics. However, there is a lower level of
knowledge about the mechanism of action of antibiotics. Only 37.1%
of respondents know that antibiotics are substances that can kill
bacteria (bactericidal antibiotics) or prevent the growth of
bacteria (bacteriostatic). Respondents have shown a fairly good
level of knowledge about antibiotics and antimicrobial resistance
(AMR) and legal frameworks. REFERENCE:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| [
Contents
] [ INDEX ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||