| |
|
|
INTRODUCTION
The primary characteristic of meteorism is the accumulation of
gases in the gastrointestinal (GI) tract, which causes a feeling of
bloating and abdominal distension. Meteorism and abdominal
distension are among the most common digestive issues that patients
experience at both primary and secondary care levels. Meteorism is a
very common symptom occurring in people of all ages, equally
prevalent in all races, and can be present in both babies and older
individuals. Approximately 15-23% of Asians and 15-30% of Americans
suffer from bloating [1,2]. In Slovenia, about 10-30% of the general
population have bloating problems [3].
This issue was highlighted in the past by the Persian physician
Avicenna in his Canon of Medicine. Avicenna used keywords such as
bloating and gases, attributing the causes of bloating to dietary
factors, inappropriate lifestyle, gastrointestinal, and other
reasons. Furthermore, Avicenna classified the causes based on the
location of origin, dividing them into the upper part of the abdomen
(stomach) and the intestinal part of the abdomen. He also listed 38
medicinal plants used as remedies. Modern scientific data support
most of the causes of bloating mentioned in Avicenna's Canon [4].
Symptoms of meteorism are even more prevalent in patients with
functional gastrointestinal disorders [5]. Meteorism is almost
invariably associated with symptoms such as bloating, distension,
and the passage of gas from the intestines. The causes of meteorism
are usually benign, such as overeating, swallowing air during meals,
or excessive fermentation in the intestinal microbiota. More
concerning causes may include bowel obstruction, kidney stones,
functional disorders related to overeating, bacterial overgrowth,
inflammatory bowel diseases, food intolerance, allergies, blunt
trauma to solid abdominal organs, peritonitis, and idiopathic
causes.
When defining functional disorders related to bloating, it is
crucial to exclude possible organic causes of symptoms, including
malignancies.
Diagnosis can involve many tests, including invasive ones, which may
pose a certain risk to the patient and a financial burden on the
healthcare system. Therefore, a step-by-step approach and targeted
treatment approach are necessary [3].
Meteorism and abdominal distension - definition of terms:
Meteorism, bloating, and distension are different terms used to
describe the same condition: increased gas in the digestive tract.
Meteorism is the medical term for this condition, while bloating and
distension are more common terms in everyday language. Bloating
refers to a feeling of tightness or fullness in the abdomen, while
distension refers to a visible increase in abdominal girth.
Flatulence is another medical term that refers to the passage of gas
from the anus.
In a healthy individual, the gastrointestinal tract usually contains
100 to 200 ml of gas, which is physiological and reflects the
dynamic process of gas formation during digestion. Gases can enter
the gastrointestinal tract during feeding (aerophagia), arise from
the breakdown of substances and bacterial fermentation. They are
eliminated during defecation, through the diffusion of gases from
the intestines into the systemic circulation, and some gases are
necessary for the metabolism of the intestinal microbiota. In
addition to causing discomfort, intestinal gases can be associated
with more serious symptoms. In the intestinal microbiota, bacteria
such as Bacteroides, Ruminococcus, Roseburia, Clostridium,
Eubacterium, Desulfovibrio, and Methanobrevibacter are among the
most common microbes responsible for the formation of intestinal
gases. More than 99% of intestinal gas consists of hydrogen, carbon
dioxide, and methane, while less than 1% consists of other odorous
compounds. Food groups associated with intestinal gases include
legumes, vegetables, fruits, cereals, and for some individuals,
dairy products. This food is rich in indigestible carbohydrates such
as oligosaccharides of the raffinose family, fructans, polyols, and
for sensitive individuals, lactose. These carbohydrates are
fermented by colonic bacteria, producing gases directly or through
cross-fermentation [8].
The composition of intestinal gases partly explains their origin:
nitrogen (N2) is usually from swallowed air; hydrogen (H2) is
produced by bacterial fermentation of carbohydrates; carbon dioxide
(CO2) is produced by bacterial fermentation of carbohydrates, fats,
and proteins; methane (CH4) is produced during anaerobic bacterial
metabolism. When there is an imbalance between gas production and
expulsion in the digestive system, it manifests as a feeling of
bloating with or without visible abdominal distension. A healthy
individual can tolerate up to 500 ml of air in the gastrointestinal
tract without major symptoms, but in patients with irritable bowel
syndrome, symptoms can be triggered by even minimal increases in gas
volume in the gastrointestinal tract [6,7].
Meteorism (bloating) is a symptom that patients describe as a
feeling of increased pressure in the abdominal cavity.
Simultaneously, abdominal distension may accompany it, wherein we
find an objectively increased volume of the abdomen; however,
abdominal distension can also occur as an independent sign [8,9].
Bloating and abdominal distension occasionally occur even in healthy
individuals as a result of normal digestion (especially after meals
rich in fats and fermentable sugars). The characteristic of
"physiological" bloating and distension is that they occur shortly
after meals, are short-lived, and disappear after urination or
passing gas. Initially, bloating and abdominal distension were only
understood as consequences of excessive air in the intestines.
Today, we know that the pathophysiology of both conditions is much
more complex and the result of different mechanisms. In addition to
increased gas production, which accumulates in the intestines along
with fluid, altered intestinal microbiota and functionally altered
enteric nervous system, which cause visceral hyperalgesia and
motility disorders [9,10].
The pathophysiology of functional gastrointestinal disorders with
meteorism and abdominal distension is multifactorial and not fully
understood. Several underlying mechanisms have been proposed that
may coexist in individual patients:
- Intraluminal content of the gut (increased gas and
fluid volume)
- Visceral hypersensitivity
- Abdominal-diaphragmatic dysenergia (Instead of the
relaxation of the diaphragm and contraction of the abdominal
walls, food intake leads to relaxation of the abdominal walls,
and the diaphragm moves lower and closer to the abdomen. This
leads to increased pressure in the abdominal cavity, which can
lead to meteorism, pain, and in some cases, constipation. ADD is
often seen together with pelvic floor muscle disinhibition.)
- Constipation
- Obesity
- Dysbiosis (leading to chronic inflammation, which
then leads to sensory and motor dysfunction)
- Psychogenic comorbidities (anxiety and depression)
[1,3]
These factors can interact and contribute to the development and
persistence of symptoms associated with meteorism and abdominal
distension.
Approach to patients with meteorism:
The etiology of meteorism and abdominal distension is highly
diverse, categorized into organic and functional causes. Diagnosis
is often demanding, prolonged, and costly.
Understanding the most common pathological conditions is essential
for the rational treatment of patients with meteorism. Patients can
be spared from many unpleasant and potentially risky examinations,
and prompt symptom improvement can be achieved through proper
disease recognition and treatment. When organic causes are ruled
out, particular attention must be paid to alarm symptoms. (Alarm
symptoms are indicators of possible organic diseases, and it is
necessary for a gastroenterologist to examine the patient as soon as
they are noticed. These symptoms include: sudden onset anemia due to
bleeding from the digestive tract, significant unintended weight
loss, persistent vomiting, difficulty swallowing, and the presence
of a palpable mass in the abdomen.) The presence of these signs with
bloating should prompt us to quickly perform endoscopic and imaging
diagnostics to rule out potential significant organic diseases.
Otherwise, endoscopic and imaging diagnostics often provide little
information when diagnosing the causes of functional meteorism
[7,10,11g.
Patient dietary habits are important in history taking. Consuming
large individual meals and fast eating can cause postprandial
bloating. Such patients are advised to eat smaller meals several
times a day. Additionally, certain foods can cause excessive
bloating: onions, legumes, coffee, carbonated beverages, or fruit
sugars [11]. In particular, these latter mentioned foods produce a
lot of gas during breakdown, which is the cause of the problem. This
knowledge formed the basis for the very popular "FODMAP" diet today.
The FODMAP diet is a dietary approach used to alleviate symptoms of
irritable bowel syndrome (IBS), which include pain, bloating,
diarrhea, and constipation. FODMAP is an acronym for fermentable
oligosaccharides, disaccharides, monosaccharides, and polyols, which
are types of carbohydrates that some people cannot digest well. The
FODMAP diet reduces the intake of these substances and can help
reduce inflammation and gas production in the intestines. The FODMAP
diet is conducted in three phases: elimination, reintroduction, and
adaptation. In the first phase, all high-FODMAP foods are
eliminated, in the second phase, they are gradually reintroduced one
by one to determine which foods cause symptoms, and in the third
phase, the diet is adjusted based on individual tolerance. The
effectiveness of a diet avoiding fermentable oligo-, di-,
monosaccharides and polyols has been demonstrated in randomized
studies in patients with irritable bowel syndrome [12,13]. Dietary
history is also important for identifying possible diseases
resulting from the harmful effects of food on the gastrointestinal
system. Among them, lactose intolerance is the most common [14]. If
problems occur after consuming gluten in the diet, celiac disease
diagnosis is necessary [15]. Exocrine pancreatic insufficiency in
older individuals is not so rare [16].
Bloating can also result from certain medications, and it is one of
the side effects of metformin, while opioid analgesics can cause
both bloating and constipation simultaneously [11]. In the case of
constipation, there is disrupted stool and gas expulsion, which then
accumulate in the digestive tract. Up to 80% of patients report
bloating symptoms when they have constipation. In most patients,
bloating symptoms will disappear after resolving constipation [17].
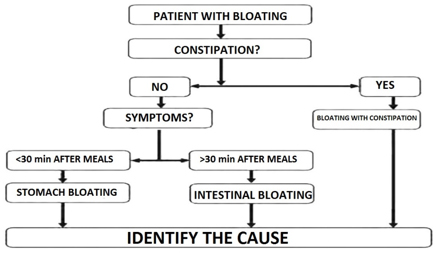
When further defining the causes of bloating, the timing of the
onset of symptoms can be helpful. If discomfort occurs shortly after
eating, the cause of bloating is usually in the upper
gastrointestinal tract – "gastric bloating." However, if a patient
reports bloating long after eating, the cause is usually lower in
the digestive tract - "intestinal bloating."
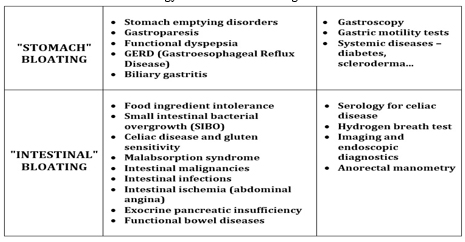
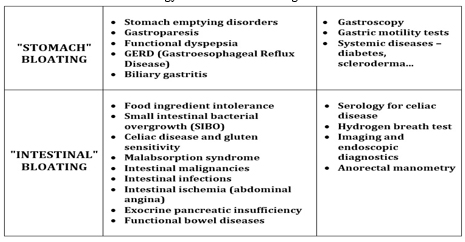
In summary: When "gastric" meteorism is present, we usually think of
disorders of gastric emptying, gastroparesis, functional dyspepsia,
GERD, or biliary gastritis. In this case, the most commonly used
diagnostic tools are gastroscopy or X-ray imaging of the upper GI
tract. If it is "intestinal" meteorism, we suspect intolerance to
food ingredients, small intestinal bacterial overgrowth (SIBO),
celiac disease and gluten sensitivity, malabsorption syndrome, bowel
malignancy, intestinal infections, bowel ischemia (abdominal
angina), exocrine pancreatic insufficiency, or functional bowel
diseases. Diagnostic procedures include serological tests for celiac
disease, hydrogen breath test, imaging and endoscopic diagnostics,
and if necessary, anorectal manometry. A simplified algorithm for
the initial treatment of meteorism is summarized in Figure 1 [3].
Figure 1. Simplified procedure for the initial
treatment of a patient with flatulence
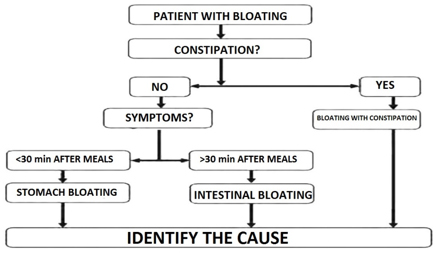
Table 1 shows some of the previously mentioned etiologically most
common conditions and common diagnostic procedures [3].
Table 1. Common etiology and some of the
diagnostic tests for flatulence
Certain more significant conditions that cause bloating
Among the more common causes of bloating are diseases due to altered
absorption of nutrients and food intolerances. The most common
causes of malabsorption can often be ruled out without invasive
interventions, even at the primary healthcare level. In recent
years, gluten-related diseases have become significant
gastrointestinal tract disorders. We must consider them, among other
reasons, because of their epidemiological dimensions. According to
some estimates, celiac disease, non-celiac gluten sensitivity, and
wheat allergy affect up to 6% of the general population, and they
all share symptoms resulting from the harmful effects of gluten.
Introducing a gluten-free diet for most patients leads to objective
and subjective improvement of the disease [14,18].
Celiac disease
Celiac disease is a condition that should always be considered in
patients with bloating. It affects 1-2% of the population and is the
most common enteropathy. Special attention must be paid to it in all
age groups, especially in patients with type 1 diabetes and
Hashimoto's thyroiditis, where a lower threshold of suspicion for
testing should be maintained [18,19]. Serological diagnostics play a
role as a screening test, with the determination of IgA antibodies
against tissue transglutaminase (IgAtTG) being the first-choice
test. Despite the high specificity and sensitivity of serological
testing, it is not sufficient for diagnosing celiac disease in
adults. Confirmation through endoscopic examination and histological
examination of duodenal mucosa biopsy is necessary for a definitive
diagnosis. All patients with positive serological findings should be
referred for endoscopic diagnosis. Regardless of the serological
test result, endoscopic diagnosis is performed in patients with a
high probability of celiac disease. Patients with symptomatic
malabsorption, unexplained diarrhea with weight loss, unexplained
iron-deficiency anemia, herpetiform dermatitis, or symptomatic
patients who are first-degree relatives of celiac disease patients
fall into this category [19]. Serological testing and endoscopic
examination must be performed in patients following a
gluten-containing diet. If the patient is on a gluten-free diet at
the time of testing, they must be gluten-loaded. Recent studies have
shown that even small amounts of gluten can induce inflammation. The
gluten challenge should last at least 2 weeks, and if the patient
tolerates the diet, it can be extended up to 6 weeks [20,21].
Genetic testing for celiac disease may be used in patients already
on a gluten-free diet to determine the presence of HLA DQ2 and DQ8
alleles, which are necessary for celiac disease development; the
absence of these alleles excludes the disease with a probability of
over 99%. However, genetic testing is not used in routine practice
and is indicated for unclear forms of celiac disease and diagnosing
refractory forms of the disease [21].
Non-celiac gluten sensitivity (NCGS) has emerged as a separate
nosological entity in recent years. Symptoms are varied and similar
to those of celiac disease and other functional gastrointestinal
disorders, associated with gluten consumption. Since the mechanism
of the disease is poorly understood, there is still no diagnostic
biomarker. Therefore, the diagnosis of non-celiac gluten sensitivity
is made by excluding celiac disease. Wheat allergy, on the other
hand, results from a classic allergic reaction (type 1
hypersensitivity) to proteins contained in wheat, including gluten.
When antigens enter the body, the allergy can affect the skin,
respiratory system, or digestive system. Gastrointestinal symptoms
are nonspecific, including bloating, distension, diarrhea, but
allergic reactions can also manifest as anaphylaxis. The diagnosis
involves excluding celiac disease through serological testing and,
if indicated, performing endoscopic examination and
histopathological examination of duodenal mucosa biopsy. Allergy to
wheat is confirmed through skin prick tests or by determining
specific antibodies [23].
A gluten-free diet is crucial in gluten-related diseases. It
involves eliminating all foods containing wheat, rye, barley, and
related grains. Compared to a normal diet, a gluten-free diet is
more expensive and less accessible. Patients must also pay close
attention to hidden sources of gluten, as it appears in various
sauces, soups, processed seafood, dried meat products, and
dressings. Additionally, the managing physician must be aware that a
gluten-free diet is not always balanced, and the patient may consume
insufficient fiber, B-complex vitamins, iron, and trace elements
(zinc, copper, selenium...) [24,25]. Celiac disease is a chronic,
lifelong condition that, if left untreated, can lead to many serious
complications (osteoporosis, the development of other autoimmune
diseases, T-cell lymphoma). Therefore, strict lifelong dietary
adherence is the cornerstone of therapy. A gluten-free diet in
patients with celiac disease reduces symptom occurrence, improves
quality of life, enhances nutritional status, and prevents disease
complications. Symptoms disappear within 2-4 weeks, serological
tests normalize within weeks to months, and the mucosa completely
regenerates after about a year. Measurement of antibodies specific
to celiac disease is the most suitable test for assessing patient
compliance with a gluten-free diet. If after 6-12 months of strict
gluten-free diet, antibody levels in blood cells normalize but the
patient still reports symptoms, further evaluation by a dietitian
and gastroenterologist is required. It is necessary to exclude
gluten contamination, refractory forms of the disease, or possible
accompanying pathology [18,20,22].
A gluten-free diet is also the foundation of treatment for
non-celiac gluten sensitivity. The goal is symptom remission and
subjective well-being of the patient. Currently, there are no clear
recommendations regarding the necessity of a lifelong gluten-free
diet in these patients. There is insufficient research on whether
non-celiac gluten sensitivity is only transient or a chronic disease
state [18].
Pancreatic exocrine insufficiency (PEI) is a common and often
overlooked cause of bloating, especially in older individuals. The
causes of pancreatic exocrine insufficiency are divided into
pancreatic or primary and non-pancreatic or secondary. In practice,
elastase determination in stool is used in diagnostics, but lately,
secretin MRCP (with much higher sensitivity and specificity) has
been employed. PEI significantly reduces the quality of life and is
diagnosed through clinical presentation and pancreatic function
tests. Treatment involves lifestyle adjustments, vitamin
supplementation, and pancreatic enzyme replacement therapy.
Long-term goals include eliminating clinical symptoms and correcting
malnutrition, addressing only the underlying disease when present.
Enzyme replacement therapy has both diagnostic and therapeutic
significance and leads to significant symptom improvement and better
quality of life for patients [26].
The treatment of meteorism and abdominal distension caused by
functional disorders, after excluding alarm signs and organic
diseases, involves gradual, individualized treatment. Patients with
mild functional bloating may only require reassurance that the
condition is benign, well, and not indicative of any
life-threatening disease.
Symptomatic treatment - Several agents are available for
treating these disorders. Antispasmodics have shown some clinical
benefit in alleviating symptoms in some patients [27]. Simethicone
has been shown to reduce the frequency and severity of meteorism,
distension, and bloating [28,29]. Peppermint oil reduced abdominal
distension compared to placebo [30,31]. Despite their popularity,
evidence is lacking regarding other commonly used agents such as
activated charcoal, Iberogast, and magnesium salts.
Dietary intervention - The role of dietary therapy in
managing bloating symptoms is crucial and is generally introduced
early in the treatment plan. The main reason for dietary therapy is
to identify foods that the patient does not tolerate and thus reduce
excessive fermentation of food residues. Initially, empirical
lactose and other poorly absorbed carbohydrate restrictions may be
implemented [12]. Alternatively, FODMAP diet or other elimination
diets may be offered to patients with meteorism and abdominal
distension if they have not improved on a restrictive diet [32].
Addressing constipation - Patients with chronic idiopathic
constipation (CIC) and irritable bowel syndrome with constipation
(IBS-C) usually report bloating in their medical history.
Lubiprostone has been found to reduce bloating in two
placebo-controlled clinical trials involving patients with IBS-C
[16,34]. Prucalopride, a selective 5-HT4 receptor agonist, enhances
spontaneous bowel movements and reduces bloating [35]. Similarly,
linaclotide, a guanylate cyclase C agonist, improves constipation
symptoms and reduces abdominal pain and bloating in patients with
CIC and IBS-C [36-42].
Microbiota modulation - Reducing gas-producing bacteria or
inducing changes in their metabolic activities may reduce excessive
fermentation and bloating. Rifaximin, a poorly absorbed
broad-spectrum antibiotic, has been found to reduce bloating and
flatulence in controlled trials in patients with and without IBS
[45,46]. Probiotics may become a therapeutic option in FABD;
however, studies have yielded different results, likely due to the
lack of standardized study methods [47,48]. A recent review
suggested that probiotics have a role in the treatment of functional
gastrointestinal disorders [49]. In a double-blind study, Ringel et
al. found that Lactobacillus acidophilus and Bifidobacterium lactis
Bi-07 reduced bloating in patients with functional gastrointestinal
disorders without constipation [50].
Abdominal biofeedback therapy - As described, postprandial
meteorism and abdominal distension may result from abnormal
relaxation of the anterior abdominal wall and diaphragmatic
contraction. It has been shown that patients can be educated to use
their abdominal and diaphragmatic muscles to reduce discomfort
associated with meteorism and abdominal distension [51].
Modulation of the brain-gut axis - If heightened perception
of bowel wall stretching and visceral hypersensitivity are key
components in the pathogenesis of functional gastrointestinal
disorders with meteorism and abdominal distension, then modulation
of the brain-gut axis appears to be a reasonable treatment option.
The efficacy of antidepressants, such as tricyclic antidepressants (TCA)
and selective serotonin reuptake inhibitors (SSRI), has been
evaluated in patients with IBS. In a small, controlled crossover
study, citalopram (SSRI) showed an increase in the number of days
without bloating after 3 and 6 weeks. In another study, desipramine
in combination with cognitive-behavioral therapy reduced bloating.
Hypnotherapy and cognitive-behavioral therapy, also offered to
patients with IBS, may be effective in patients with functional
gastrointestinal disorders [55].
CONCLUSION
Meteorism and abdominal distension represent a common clinical
problem. Like any other health condition, the clinical assessment of
gastrointestinal disorders with meteorism and abdominal distension
begins with a detailed medical history, physical examination, and
appropriate diagnostic tests. It is crucial to exclude any organic
cause of bloating and distension. Alarm symptoms, which may indicate
more serious pathology, should not be overlooked. Depending on the
frequency, gluten-related diseases should always be considered, and
in the elderly, pancreatic exocrine insufficiency should also be
considered. Celiac disease can be sufficiently excluded with
serological testing, even at the level of primary or secondary
medical facilities. In treatment, a gradual, multidisciplinary,
individualized approach is desirable. Therapy may target bowel
motility, muscle tone, microbiota, visceral sensitivity, nutrition,
and/or psychological comorbidities. Additionally, an "ex juvantibus"
response to treatment – improvement of symptoms with pancreatic
enzyme replacement therapy – indicates pancreatic exocrine
insufficiency.
LITERATURA:
- Lacy BE, Gabbard SL, Crowell MD. Pathophysiology,
evaluation, and treatment of bloating: hope, hype, or hot air?
Gastroenterol Hepatol (N Y). 2011;7(11):729-39.
- Tuteja AK, Talley NJ, Joos SK, Tolman KG, Hickam
DH.Abdominal bloating in employed adults: prevalence,
riskfactors, and association with other bowel disorders. Am
JGastroenterol 2008;103:1241–48.
- Rado Janša Meteorizem, abdominalna distenzija,flatulenca
Gastroenterolog 2018;suplement 3:32–38.
- Naseri M, Babaeian M, Ghaffari F, Kamalinejad M, Feizi A, et
al. Bloating: Avicenna's Perspective and Modern Medicine. J Evid
Based Complementary Altern Med. 2016;21(2):154-9.
- Iovino P, Bucci C, Tremolaterra F, Santonicola A,
ChiarioniG. Bloating and functional gastro-intestinal disorders:
Whereare we and where are we going? World J
Gastroenterol.2014;20:14407–19.
- Mutuyemungu E, Singh M, Liu S, RoseDJ. Intestinal gas
production by the gut microbiota: A review Journal of Functional
Foods Volume 100, January 2023.Dostupno
na:https://www.sciencedirect.com/science/article/pii/S1756464622004376
preuzeto 22.02.2024)
- Serra J, Azpiroz F, Malagelada JR: Impaired transit and
tol-erance of intestinal gas in the irritable bowel syndrome.
Gut2001;48:14–19.
- Malagelada JR, Accarino A, Azpiroz F. Bloating andAbdominal
Distension: Old Misconceptions and CurrentKnowledge. The
American Journal of Gastroenterology. 2017;112:1221–31.
- Drossman DA . Functional gastrointestinal disorders:
history,pathophysiology, clinical features, and rome
IV.Gastroenterology 2016;150:1262–79.
- Lacy E et all Management of Chronic Abdominal Distension and
Bloating Clinical Gastroenterology and Hepatology CrossrefDOI
link:https://doi.org/10.1016/j.cgh.2020.03.056. Published Print:
2021-02
- Cotter TG, Gurney M, Loftus CG. Gas and Bloating—Controlling
Emissions. Mayo Clinic Proceedings 2016; 91:1105–13.
- Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG.A diet
low in FODMAPs reduces symptoms of irritablebowel syndrome.
Gastroenterology 2014;146:67–9.
- Böhn L, Störsrud S, Liljebo T, Collin L, Lindfors P,Törnblom
H, et al. Diet low in FODMAPs reduces symptomsof irritable bowel
syndrome as well as traditional dietaryadvice: a randomized
controlled trial. Gastroenterology2015;149:1399–407.
- Deng Y, Misselwitz B, Dai N, Fox M. Lactose Intolerance
inAdults: Biological Mechanism and Dietary Management.Nutrients
2015;7:8020–35.
- Sapone A, Bai JC, Ciacci C, et al. Spectrum of
gluten-relateddisorders: consensus on new nomenclature and
classifica-tion. BMC Medicine 2012; 10:13.
- Löhr M, Oliver M, Frulloni L. Synopsis of recent
guidelineson pancreatic exocrine insufficiency. United
EuropeanGastroenterology Journal 2013; 1:279–83.
- Iovino P, Bucci C, Tremolaterra F, Santonicola A,
ChiarioniG. Bloating and functional gastro-intestinal disorders:
Whereare we and where are we going? World J Gastroenterol.2014;
20: 14407–19.
- Elli L, Branchi F, Tomba C, et al. Diagnosis of
glutenrelated disorders: Celiac disease, wheat allergy and
non-celiac gluten sensitivity. World J Gastroenterol 2015;
21:7110–19.
- Snyder MR, Murray JA. Celiac disease: advances in
diagnosis.Expert Review of Clinical Immunology. 2016; 12:
449–63.
- Leffler D, Schuppan D, Pallav K, Najarian R, GoldsmithJD,
Hansen J, et al. Kinetics of the histological, serologicaland
symptomatic responses to gluten challenge in adultswith coeliac
disease. Gut 2013; 62: 996–1004.
- Kaswala DH, Veeraraghavan G, Kelly CP, Leffler DA.
CeliacDisease: Diagnostic Standards and Dilemmas. Diseases2015;
3: 86–101.
- Elli L, Villalta D, Roncoroni L, Barisani D, Ferrero
S,Pellegrini N, et al. Nomenclature and diagnosis of
gluten-related disorders: A position statement by the
ItalianAssociation of Hospital Gastroenterologists and
Endoscopists(AIGO). Digestive and Liver Disease 2017; 49:
138–46.
- Pasha I, Saeed F, Sultan MT, Batool R, Aziz M, Ahmed W.Wheat
Allergy and Intolerence; Recent Updates andPerspectives.
Critical Reviews in Food Science and Nutrition2016; 56: 13–24.
- Krigel A, Lebwohl B Nonceliac Gluten Sensitivity. Advancesin
Nutrition: An International Review Journal. 2016; 7:1105–10.
- Mulder CJJ, van Wanrooij RLJ, Bakker SF, Wierdsma N,Bouma G.
Gluten-Free Diet in Gluten-Related DisordersDigestive Diseases.
2013; 31: 57-62.
- Mari, A., Abu Backer, F., Mahamid, M. et al. Bloating and
Abdominal Distension: Clinical Approach and Management. Adv
Ther2019;36: 1075–1084.
- Barba E, Quiroga S, Accarino A, et al. Mechanisms of
abdominal distension in severe intestinal dysmotility:
abdomino-thoracic response to gut retention. Neurogastroenterol
Motil. 2013;25(6):e389–e394. doi: 10.1111/nmo.12128. )
- Maxton DG, Whorwell PJ. Abdominal distension in irritable
bowel syndrome: the patient’s perception. Eur Hepatol.
1992;4:241–243.
- Lewis M. Ambulatory abdominal inductance plethysmography:
towards objective assessment of abdominal distension in
irritable bowel syndrome.Gut. 2001;48(2):216–220. doi:
10.1136/gut.48.2.216.
- Dukowicz AC, Lacy BE, Levine GM. Small intestinal bacterial
overgrowth: a comprehensive review. Gastroenterol Hepatol.
2007;3:112–122.
- Bernstein J, Kasich A. A double-blind trial of simethicone
in functional disease of the upper gastrointestinal tract. J
Clin Pharmacol.1974;14(11):617–623. doi:
10.1002/j.1552-4604.1974.tb01382.x.
- Liu J, Chen G, Yeh H, Huang C, Poon S. Enteric-coated
peppermint-oil capsules in the treatment of irritable bowel
syndrome: a prospective, randomized trial. J Gastroenterol.
1997;32(6):765–768. doi: 10.1007/BF02936952.
- Cappello G, Spezzaferro M, Grossi L, Manzoli L, Marzio L.
Peppermint oil (Mintoil®) in the treatment of irritable bowel
syndrome: a prospective double blind placebo-controlled
randomized trial. Dig Liver Dis. 2007;39(6):530–536. doi:
10.1016/j.dld.2007.02.006.
- Halmos E, Power V, Shepherd S, Gibson P, Muir J. A diet low
in FODMAPs reduces symptoms of irritable bowel syndrome.
Gastroenterology.2014;146(1):67–75. doi:
10.1053/j.gastro.2013.09.046.
- Catassi G, Lionetti E, Gatti S, Catassi C. The low FODMAP
diet: many question marks for a catchy acronym. Nutrients.
2017;9(3):292. doi: 10.3390/nu9030292. (PMC free article)
- Camilleri M, Bharucha A, Ueno R, et al. Effect of a
selective chloride channel activator, lubiprostone, on
gastrointestinal transit, gastric sensory, and motor functions
in healthy volunteers. Am J Physiol Gastrointest Liver Physiol.
2006;290(5):G942–G947. doi: 10.1152/ajpgi.00264.2005.
- Tack J, Stanghellini V, Dubois D, Joseph A, Vandeplassche L,
Kerstens R. Effect of prucalopride on symptoms of chronic
constipation. Neurogastroenterol Motil. 2013;26(1):21–27. doi:
10.1111/nmo.12217.
- Castro J, Harrington A, Hughes P, et al. Linaclotide
inhibits colonic nociceptors and relieves abdominal pain via
guanylate cyclase-C and extracellular cyclic guanosine
3′,5′-monophosphate. Gastroenterology.2013;145(6):1334–1346.e11.
doi: 10.1053/j.gastro.2013.08.017.
- Limbo AJ, Schneier HA, Shiff SJ, et al. Two randomized
trials of linaclotide for chronic constipation. N Engl J Med.
2011;365:527–536. doi: 10.1056/NEJMoa1010863.
- Lacy BE, Schey R, Shiff SJ, et al. Linaclotide in chronic
idiopathic constipation patients with moderate to severe
abdominal bloating: a randomized, controlled trial. PLoS One.
2015;10:e0134349. doi: 10.1371/journal.pone.0134349.
- Videlock E, Cheng V, Cremonini F. Effects of linaclotide in
patients with irritable bowel syndrome with constipation or
chronic constipation: a meta-analysis. Clin Gastroenterol
Hepatol. 2013;11(9):1084–1092.e3. doi:
10.1016/j.cgh.2013.04.032.
- Caldarella M, Serra J, Azpiroz F, Malagelada J. Prokinetic
effects in patients with intestinal gas retention.
Gastroenterology. 2002;122(7):1748–1755. doi:
10.1053/gast.2002.33658
- Accarino A, Perez F, Azpiroz F, Quiroga S, Malagelada J.
Intestinal gas and bloating: effect of prokinetic stimulation.
Am J Gastroenterol.2008;103(8):2036–2042. doi:
10.1111/j.1572-0241.2008.01866.x.
- Pimentel M, Lembo A, Chey W, et al. Rifaximin therapy for
patients with irritable bowel syndrome without constipation. N
Engl J Med.2011;364(1):22–32. doi: 10.1056/NEJMoa1004409.
- Sharara A, Aoun E, Abdul-Baki H, Mounzer R, Sidani S, ElHajj
I. A randomized double-blind placebo-controlled trial of
rifaximin in patients with abdominal bloating and flatulence. Am
J Gastroenterol.2006;101(2):326–333. doi:
10.1111/j.1572-0241.2006.00458.x.
- Moayyedi P, Ford A, Talley N, et al. The efficacy of
probiotics in the treatment of irritable bowel syndrome: a
systematic review. Gut. 2008;59(3):325–332. doi:
10.1136/gut.2008.167270.
- Jonkers D, Stockbrügger R. Review article: probiotics in
gastrointestinal and liver diseases. Aliment Pharmacol Ther.
2007;26:133–148. doi: 10.1111/j.1365-2036.2007.03480.x.
- Ringel Y, Carroll I. Alterations in the intestinal
microbiota and functional bowel symptoms. Gastrointest Endosc
Clin N Am. 2009;19(1):141–150. doi: 10.1016/j.giec.2008.12.004.
- Ringel-Kulka T, Palsson O, Maier D, et al. Probiotic
bacteria Lactobacillus acidophilus NCFM and Bifidobacterium
lactis bi-07 versus placebo for the symptoms of bloating in
patients with functional bowel disorders. J Clin
Gastroenterol.2011;45(6):518–525. doi:
10.1097/MCG.0b013e31820ca4d6.
- Barba E, Burri E, Accarino A, et al. Abdominothoracic
mechanisms of functional abdominal distension and correction by
biofeedback. Gastroenterology.2015;148(4):732–739. doi:
10.1053/j.gastro.2014.12.006. (PubMed)
- Tack J. A controlled crossover study of the selective
serotonin reuptake inhibitor citalopram in irritable bowel
syndrome. Gut.2005;55(8):1095–1103. doi:
10.1136/gut.2005.077503.
- Rahimi R, Nikfar S, Abdollahi M. Efficacy and tolerability
of Hypericum perforatum in major depressive disorder in
comparison with selective serotonin reuptake inhibitors: a
meta-analysis. Prog Neuropsychopharmacol Biol
Psychiatry.2009;33(1):118–127. doi: 10.1016/j.pnpbp.2008.10.018.
- Drossman D, Toner B, Whitehead W, et al.
Cognitive-behavioral therapy versus education and desipramine
versus placebo for moderate to severe functional bowel
disorders. Gastroenterology.2003;125(1):19–31. doi:
10.1016/S0016-5085(03)00669-3.
- Schmulson M, Chang L. Review article: the treatment of
functional abdominal bloating and distension. Aliment Pharmacol
Ther.2011;33(10):1071–1086. doi:
10.1111/j.1365-2036.2011.04637.x.
|
|
|
|