| |
|
|
INTRODUCTION
The term "melanonychia" derives from the Greek words "Melas,"
meaning black or brown color, and "Onyx," meaning nail. It is
characterized by black-brown discoloration of the nail plate and
nail matrix epithelium caused by the accumulation of melanin. It can
affect one or more nail plates, both on the hands and feet. It
predominantly presents as a longitudinal black-brown streak starting
from the matrix and extending to the free edge of the nail plate.
Less commonly, the discoloration affects the entire nail plate or
manifests as a transverse band.
The black-brown discoloration is caused by the accumulation of
melanin produced by melanocytes in the nail matrix. Differentiation
includes simple melanocyte activation, benign, and malignant
melanocyte proliferation. Melanocyte activation can be induced by
iatrogenic agents, pathogenic microorganisms, nutritional deficits,
and trauma. Additionally, it can be present in certain physiological
conditions, abnormalities of the nail plate or periungual tissue,
dermatological conditions, tumors, systemic disorders, and
syndromes. Melanocyte proliferation includes lentigo, nail matrix
nevus, and subungual melanoma.
Melanonychia in childhood is rare. In adults, its prevalence varies
(from 0.8% to 23%). Diagnosis is based on history, physical
examination, onychoscopic examination, and biopsy with histological
examination. Treatment depends on the etiology and nature of
melanonychia.
CASE REPORT
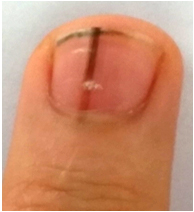
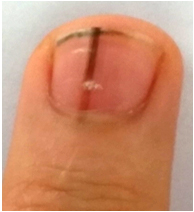
During a systematic examination of a 13-year-old boy, a single
black-brown, linear discoloration was observed on the index finger
of his left, non-dominant hand (See Figure 1). There was no nail
plate dystrophy, periungual pigmentation, or bleeding. The onset
time of the change could not be determined. The boy was healthy, and
his medical and family history were unremarkable. On onychoscopic
examination, brown-black, parallel, longitudinal lines were observed
on a brown background. The hyperpigmentation of the nail bed was
visible through a thin cuticle and the distal part of the proximal
nail fold. A diagnosis of nail matrix nevus was made, and regular
follow-up by a dermatologist was advised.
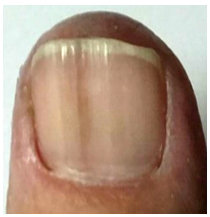
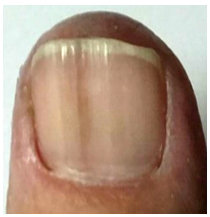
During a follow-up examination of a 59-year-old female patient, a
single melanonychia of the nail plate of the thumb of her right,
dominant hand was observed. It was a brown, linear, uniformly
pigmented, clearly demarcated discoloration with discreetly
irregular edges from the proximal nail fold to the free edge of the
nail plate. There were no signs of trauma, nail plate dystrophy, or
bleeding. The change had been present for several months without
altering in size or pigment intensity. The patient, a homemaker and
non-smoker, had cardiomyopathy, irregular heart rhythm, high blood
pressure, type 2 diabetes, and high cholesterol levels. She was on
continuous therapy with 200mg of amiodarone, 4mg of acenocoumarol,
20mg of enalapril, 1000mg of metformin, and 10mg of rosuvastatin. On
onychoscopic examination, brown-black longitudinal lines of varying
width were visible through the cuticle and proximal nail fold on a
brown background. A longitudinal excision biopsy was indicated,
revealing an increased number of heavily pigmented melanocytes
without signs of atypia in the basal epidermis. Thus, a diagnosis of
nail plate lentigo was made, and the patient was advised regular
dermatologist check-ups.
| Figure 1. Nail matrix nevus |
Figure 2. Lentigo of the nail
matrix |
 |
 |
DISCUSSION
Melanonychia implies nail pigmentation caused by simple
activation of nail matrix melanocytes, either benign (lentigo or
nail matrix nevus) or malignant (subungual melanoma) proliferation
of the same [1].
Simple melanocyte activation (melanocyte stimulation, functional
melanonychia) involves increased melanin production in secondarily
activated melanocytes without an increase in the number of
melanocytes [4].
Melanocytes are physiologically activated in ethnic melanonychia and
pregnancy [7]. Ethnic melanonychia is predominantly present in
individuals with darker pigmented skin types IV, V, and VI [1,7].
Its prevalence varies from 1% in Caucasians, 10%-20% in Asians, to
77–100% in African Americans [7]. It is most commonly found on the
thumb and index finger of the hand and the big toe [1,7]. It often
affects multiple nail plates, and its width increases with age
[1,7]. Melanocyte activation during pregnancy involves several nails
on the hands and/or feet [1]. It may disappear or persist after
childbirth [1].
Melanocyte activation caused by drugs is often accompanied by skin
and/or mucous membrane pigmentation [1]. Its form is variable
(transverse or longitudinal stripes, solitary or associated) [1].
The majority of transverse melanonychias are caused by drugs [1].
Often, the changes involve several nails and fade partially or
completely upon discontinuation of the drug [1,3]. Melanonychia can
be caused by antiretroviral drugs (lamivudine, zidovudine),
antimalarial drugs (mepacrine, amodiaquine, chloroquine, quinacrine),
anticancer drugs (cyclophosphamide, doxorubicin, hydroxyurea,
busulfan, taxanes, capecitabine, cisplatin, bleomycin, daunorubicin,
dacarbazine, 5-fluorouracil, methotrexate) as well as simultaneous
use of antiplatelet and anticoagulant drugs [1,2,3].
Melanocyte activation can also be induced by metals (arsenic,
thallium, mercury), biological agents (clofazimine, infliximab,
psoralen, phenytoin, fluconazole, cyclines, ketoconazole,
phenothiazines), ultraviolet therapy, electron beam therapy, and
conventional radiographic therapy (used in the 1950s and 1960s)
[1,3]. The same effect is produced by henna, tobacco, potassium
permanganate, tar, and silver nitrate [1].
Fungal melanocyte activation occurs as a result of onychomycosis,
fungal infection of the nail plate [9]. So far, at least 21
different species of fungi that can cause fungal melanonychia have
been described [9]. Its form is variable [1]. Dermatophytes (Scytalidium
dimidiatum) form longitudinal stripes, yeasts (Candida albicans,
Candida humicola, Candida parapsilosis) and molds (Trichophyton
rubrum, Alternaria, Exophiala) form diffuse discoloration [9,10].
With eradication of the causative agent, the appearance of the nail
plate usually normalizes [10,11]. The recurrence rate ranges from
10% to 50% [11].
Melanonychia can also be caused by gram-negative bacteria, including
Pseudomonas aeruginosa, Escherichia coli, and Proteus mirabilis
[1,12,13]. Immunocompromised states and working in a moist
environment are risk factors [1]. Longitudinal stripes with a wider
proximal edge or diffuse discolorations starting from the junction
of the proximal and lateral nail folds and spreading irregularly
along the medial edge are present on the nail plates [1].
The human immunodeficiency virus (HIV) predisposes to melanonychia
(diffuse discoloration, multiple longitudinal or transverse stripes
on multiple nail plates) accompanied by hyperpigmentation of the
mucous membranes, palms, and soles [14].
Dark brown discoloration of the nail plate is observed in
malnutrition (predominantly protein deficiency and vitamin D
deficiency) [1,15]. It is also present in the absence of vitamin B12
(often found in vegetarians) due to decreased glutathione
concentration and subsequent inhibition of tyrosinase, the main
enzyme of melanogenesis [16].
Repeated local trauma caused by uncomfortable footwear, occupational
trauma, onychophagia, onychotillomania, or carpal tunnel syndrome
can activate nail matrix melanocytes [1,13]. Traumatic melanonychia
is often accompanied by periungual signs of trauma [1]. Nail matrix
melanocytes are often activated in a variety of inflammatory
conditions and skin tumors, including Lichen planus, chronic
paronychia, psoriasis, amyloidosis, chronic radiation dermatitis,
Hallopeau acrodermatitis, myxoid pseudocyst, localized scleroderma,
onychomatrix, subungual linear keratosis, Verruca vulgaris,
subungual fibrous histiocytoma, Bowen's disease, basal cell
carcinoma, subungual fibrous histiocytoma [1,13,14].
Multiple dark brown stripes or diffuse discoloration on multiple
nail plates on the hands and feet are observed in Addison's disease,
Cushing's syndrome, hyperthyroidism, acromegaly, alkaptonuria,
hemosiderosis, hyperbilirubinemia, and porphyria [1]. Melanocyte
activation is also present in the host reaction against
transplantation (Graft versus host disease, GVHD) [1].
Laugier-Hunziker, Peutz-Jeghers, and Touraine syndromes are
characterized by multiple dark brown stripes on the nail plates
accompanied by pigmented mucous membrane macules on the lips and
oral cavity [1,3]. Laugier-Hunziker syndrome occurs sporadically in
white adults aged 20 to 40 years [1,3,18]. It does not have systemic
manifestations or malignant potential [1,3,18]. Peutz-Jeghers and
Touraine syndromes are predominantly present in children and are
inherited in an autosomal dominant manner [1,3,18]. They are
associated with intestinal polyps and an increased risk of
gastrointestinal and pancreatic malignancies [1,3,18].
Melanocytic hyperplasia involves an increase in the number of
melanocytes within the nail matrix [19,20]. We distinguish lentigo,
nail matrix nevus, and subungual melanoma [19,20].
Lentigo and nail matrix nevus are benign changes [20]. Lentigo is
melanocytic hyperplasia in the absence of melanocytic nests, usually
present in adults (9% of longitudinal melanonychias in adults)
[1,20]. Nail matrix nevus contains at least one melanocytic nest
[19,20]. It accounts for 12% of longitudinal melanonychias in adults
and 48% of longitudinal melanonychias in children [1]. We
distinguish congenital and acquired nevus [20]. In children,
especially under the age of 3, it is difficult to determine whether
the nevus is congenital or acquired, considering that nail matrix
nevus in the early stage can present as a colorless stripe [20].
In situ and invasive subungual melanoma belong to malignant
melanocytic hyperplasias [3]. Subungual melanoma is a rare form of
melanoma (1-3% of melanomas) [1]. The incidence varies among
different races (from 10% to 25%), with higher incidences observed
in Asian countries including Japan, China, and Korea [1]. There is
no significant difference in incidence by gender [20]. The peak
incidence is between the ages of 50 and 70 years [20]. Subungual
melanoma is usually localized on the thumb, big toe, and middle toe
[20]. In 38%-76% of cases, longitudinal melanonychia represents the
first manifestation of the disease [20].
The medical history includes gender, age, occupation, hobbies,
previous trauma, medical history, family medical history, continuous
therapy, time of onset of melanonychia, location of melanonychia,
color and width of the pigment strip, nail pain and/or bleeding, and
nail deformity/brittleness [20]. In pregnant women, it includes a
history of pregnancy and the relationship between pregnancy and the
onset or progression of melanonychia [20].
The physical examination requires careful assessment of all twenty
nails, skin, and mucous membranes [3]. During this examination, it
is necessary to determine the following:
- Is one or more nails involved?
- Does one nail differ from the others (if multiple nails are
involved)?
- Is the discoloration present on the surface, within, or beneath
the nail plate?
- Is the discoloration linearly oriented?
- Is the discoloration wider or darker proximally?
- Is the discoloration associated with nail plate dystrophy
(abrasion, splitting, cracking), periungual pigmentation, and
bleeding?
- Is the discoloration accompanied by changes in the skin and mucous
membranes? [1,3]
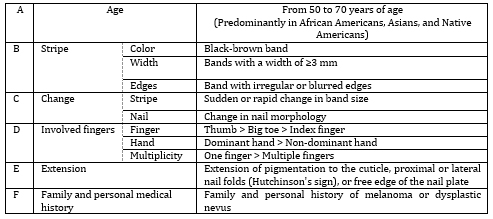
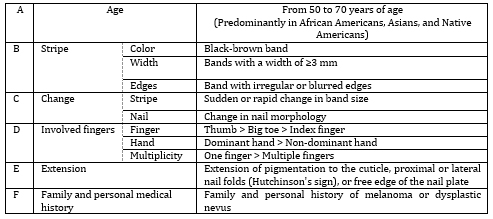
In the identification of subungual melanoma, the "ABCDE" (from
English: Age, Nail band, Change, Digit involved, Extension, Family)
rule established in 2000 by Levi and colleagues is applied (Table
1.) [20].
Table 1. ABCDEF rule of identification of
subungual melanoma
Nail plate onychoscopy (with handheld dermoscope and digital
videodermoscope) enables differentiation between melanin and
non-melanin pigmentation (subungual hematoma, pigmentation caused by
exogenous substances) [1,20]. Subungual hematoma is characterized by
beads of varying sizes and colors (ranging from bright red to brown
or black) depending on the depth and duration of bleeding [1]. It is
important to note that subungual bleeding does not exclude the
presence of subungual melanoma [1]. Additionally, Hutchinson's sign
(extension of pigmentation into the cuticle, proximal, or lateral
nail folds) of subungual melanoma and pseudo-Hutchinson's sign (hyperpigmentation
of the nail bed visible through the thin cuticle and distal part of
the proximal nail fold) should be distinguished [20,21].
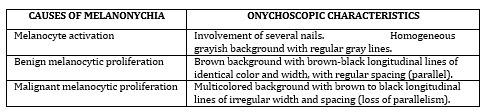
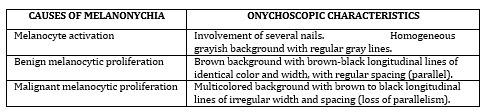
Onychoscopic patterns of melanocyte activation, benign, and
malignant proliferation have been convincingly confirmed in
scientific research (Table 2) [1,20,22].
Table 2. Onychoscopic characteristics in relation
to the cause of melanonychia 1
Intraoperative onychoscopy of the nail bed and matrix allows
direct visualization of the changes in the nail bed and matrix [1].
Additionally, it facilitates determining margins and complete
excision of the lesion [22].
Biopsy represents the gold standard in the diagnosis of subungual
melanoma [6]. The type and location of the biopsy are determined by
the morphological characteristics of melanonychia [1].
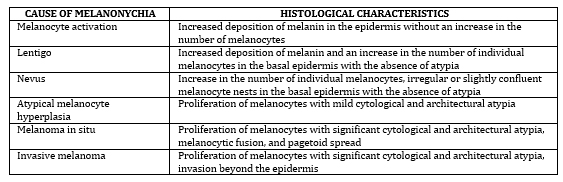
Histologically, subungual melanoma is characterized by asymmetry,
infiltrative edges, significantly increased number of melanocytes in
the basal layer (up to 39-136/mm), tendency to form compact
aggregates in the suprabasal layers, presence of cytological atypia,
and inflammatory processes [13]. Malignant melanocytes are
multi-nucleated with large, atypical nuclei, exhibiting increased
mitotic activity (Table 3).
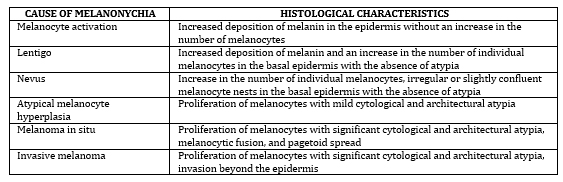
Table 3. Histological characteristics in relation
to the cause of melanonychia
CONCLUSION
Melanonychia represents a complex clinical entity whose etiology
is often not easily determined. Simple activation of the nail matrix
melanocytes, lentigo, nevus, and subungual melanoma have similar
clinical characteristics, but their prognoses vary significantly.
Careful medical history, physical examination, onychoscopic
examination, and ultimately biopsy with histological examination
allow for early diagnosis of subungual melanoma as a fundamental
goal and precondition for successful treatment of the disease.
LITERATURE:
- Singal A, Bisherwal K. Melanonychia: Etiology, Diagnosis,
and Treatment. Indian Dermatol Online J. 2020;11(1):1-11.
Dostupno
na:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7001389/
- Tosti A. Diseases of Hair and Nails. 450-Diseases of Hair
and Nails. Editors: Lee Goldman L, Schafer AI. Goldman's Cecil
Medicine (Twenty Fourth Edition). Saunders WB.2012:2551-2556.
Dostupno na:
https://www.sciencedirect.com/topics/medicine-and-dentistry/melanonychia
- Jefferson J, Rich P. Melanonychia. Dermatology Research and
Practice. 2012;952186. Dostupno na:
https://doi.org/10.1155/2012/952186
- Güneş P, Göktay F. Melanocytic Lesions of the Nail Unit.
Dermatopathology (Basel). 2018;5(3):98-107. Dostupno na:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6120410/
- Putri HA.A Case of Longitudinal Melanonychia in A Child:
Benign or Malignant? J Gen Proced Dermatol Venereol Indones.
2022:6(2);51-56. Dostupno na:
https://scholarhub.ui.ac.id/cgi/viewcontent.cgi?params=/context/jdvi/article/1008/&path_info=9._CR_A_Case_of_Longitudinal_Melanonycia_
on_child__Benign_or_Malign_FINAL.pdf
- Quiroz Alfaro AJ, Greiffenstein J, Herrera Ortiz AF, Dussan
Tovar CA, Saldarriaga Santamaría S, Cifuentes Burbanoet J et al.
Incipient Melanonychia: Benign Finding or Occult Malignancy? A
Case Report of Subungual Melanoma. Cureus. 2023; 15(1):e34292.
Dostupno na:
https://www.cureus.com/articles/134276-incipient-melanonychia-benign-finding-or-occult-malignancy-a-case-report-of-subungual-melanoma#!/
- Lee DK, Lipner SE. Optimal diagnosis and management of
common nail disorders. Annals of Medicine.2022;54(1):694-712.
Dostupno na:
https://www.tandfonline.com/doi/full/10.1080/07853890.2022.2044511
- Cristián Fischer L, Matías Sanhueza M. Hiperpigmentación
cutánea y melanoniquia provocada por hidroxicloroquina: primer
caso reportado en Chile. Actas Dermosifiliogr. 2020. Dostupno
na: https://doi.org/10.1016/j.ad.2019.02.027
- Elmas ÖF, Metin MS. Dermoscopic findings of fungal
melanonychia. Postepy Dermatol Alergol. 2020;37(2):180-183.
Dostupno na:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262796/
- Cohen PR, Shurman J. Fungal Melanonychia as a Solitary Black
Linear Vertical Nail Plate Streak: Case Report and Literature
Review of Candida-Associated Longitudinal Melanonychia Striata.
Cureus. 2021;13(4):e14248. Dostupno na:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8093122/
- Westerberg DP, Voyack MJ. Onychomycosis: Current trends in
diagnosis and treatment. Am Fam Physician. 2013;88(11):762-70.
Dostupno na:
https://www.aafp.org/pubs/afp/issues/2013/1201/p762.html
- Wu KY, Suh GA, Shi AY. Chronic Polymicrobial Infectious
Melanonychia Striata. JBJS case connector.2013;13(2). Dostupno
na:
https://mayoclinic.elsevierpure.com/en/publications/chronic-polymicrobial-infectious-melanonychia-striata
- Gradinaru TC, Mihai M, Beiu C, Tebeica T, Giurcaneanu C.
Melanonychia - Clues for a Correct Diagnosis. Cureus.
2020;12(1):e6621. Dostupno na:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7008765/
- Visuvanathan VV, Koh KC. Dark fingernails. Malays Fam
Physician. 2015;10(3):40-2. Dostupno na:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4992355/
- Seshadri D, De D. Nails in nutritional deficiencies. Indian
J Dermatol Venereol Leprol 2012;78:237-241. Dostupno na:
https://ijdvl.com/nails-in-nutritional-deficiencies/
- Afra TP, Razmi TM, Narang T. Reversible Melanonychia
Revealing Nutritional Vitamin-B12 Deficiency. Indian Dermatol
Online J. 2020;11(5):847-848. Dostupno na:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7678521/
- Lalitha C, Shwetha S, Asha G S.Assessment of clinical and
etiological factors in nail dyschromias.Indian Journal of
Clinical and Experimental Dermatology 2021;7(4):324–330.
Dostupno na: https://www.ijced.org/html-article/15411
- Wang WM, Wang X, Duan N, Jiang HL, Huang XF.
Laugier–Hunziker syndrome: a report of three cases and
literature review. Int J Oral Sci.2012;4:226–230. Dostupno na:
https://doi.org/10.1038/ijos.2012.60
- Aseri J, Kumawat K, Tamta A, Bhargava P, Meena RS. Basic
approach to melanonychia: a review.Int J Res Dermatol.
2022;8(4):426-432. Dostupno na:
https://www.ijord.com/index.php/ijord/article/view/1566
- Cao Y, Han D.Longitudinal Melanonychia: How to Distinguish a
Malignant Condition from a Benign One. CJPRS. 2021;3(1):56-62.
Dostupno na:
https://www.sciencedirect.com/science/article/pii/S2096691121000807
- Zhu M, Wang S, Wang P. Melanonychia with pseudo-Hutchinson
sign may assist in diagnosis of Addison's disease. Skin Res
Technol. 2023;29(8):e13441.Dostupno na:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10427615/
- Di Chiacchio N, Hirata SH, Enokihara MY, Michalany NS,
Fabbrocini G, Tosti A. Dermatologists' Accuracy in Early
Diagnosis of Melanoma of the Nail Matrix. Arch Dermatol.
2010;146(4):382–387. Dostupno na:
https://jamanetwork.com/journals/jamadermatology/fullarticle/421241
- Anindya PH, Ennesta A, Qaira A. A Case of Longitudinal
Melanonychia in A Child: Benign or Malignant? Journal of
General-Procedural Dermatology & Venereology Indonesia.
2022;6(2):51-56. Dostupno na:
https://scholarhub.ui.ac.id/jdvi/vol6/iss2/9?utm_source=scholarhub.ui.ac.id%2Fjdvi%2Fvol6%2Fiss2%2F9&utm_medium=PDF&utm_campaign=PDFCoverPages
|
|
|
|