| |
Preuzmite
rad u pdf formatu |
|
Sažetak: Uvod:
Bilateralni talamički infarkti su retki i obično udruženi sa
tipičnom kliničkom slikom koja, pored ostalog, uključuje i
neuropsihološke promene. Prikaz slučaja: Prikazan je slučaj
tridesetsedmogodišnje žene sa akutno nastalim diplopijama usled
„skew” devijacije, centralnom desnostranom parezom mimične
muskulature, levostranom hemihipestezijom, ataksijom, sa očuvanim
nivoom svesti i bez ikakvih neuropsiholoških smetnji, izuzev blagog
memorijskog deficita. Postavljena je dijagnoza bilateralnog
talamičkog infarkta uzrokovanog kardioembolizacijom preko
perzistentnog foramena ovale. Zaključak: U slučajevima bilateralnog
talamičnog infarkta može se pretpostaviti postojanje retke anatomske
varijante talamičke perfuzije poznate kao Percheronova arterija,
jedinstvenog stabla koje se grana za irigaciju oba paramedijalne
talamičke zone. Uzrok infarkta može biti kardioembolizacija kroz
perzistentni foramen ovale, naročito kod mladih ljudi. Naš slučaj
prikazuje kombinaciju dva specifična patološka stanja –
perzistentnog foramena ovale i bilateralnog talamičkog infarkta.
Klinička prezentacija u ovom slučaju je atipična za bilateralni
paramedijalni infarkt.
Ključne reči: bilateralni talamički infarkt, „skew”
devijacija, perzistentni foramen ovale, Percheronova arterija.
Summary: Background: Simultaneous bilateral thalamic
infarctions are rare and in most cases associated with typical
clinical pattern which, beside other things, include
neuropsychological changes. Case report: We report a case of a 37-
year-old woman with acute onset ofdiplopia from skew deviation,
right-sided central facial nerve palsy, left hemihypesthesia,
ataxia, with normal level of consciousness and without any
neuropsychological disturbances except minor memory deficit. She was
diagnosed with bilateral thalamic infarction due to the
cardioembolisation via patent foramen ovale. Conclusion: In cases of
bilateral thalamic infarction one can presume the existence of rare
anatomic variant of thalamic perfusion commonly known as the artery
of Percheron, single artery trunk that branches to irrigate both
paramedian territories of thalamus. The cause of infarction can be
cardioembolism trough the patent foramen ovale, especially in young
adults. Our case represents a combination of two specific
pathological conditions – patent foramen ovale and bilateral
thalamic infarction. Clinical presentation in this case was unusual
for the bithalamic paramedian infarction.
Key words: bilateral thalamic infarction, skew deviation,
patent foramen ovale, artery of Percheron |
|
|
|
| |
|
|
INTRODUCTION
Simultaneous bilateral thalamic infarctions are rare,
representing approximately 0.6% of all ischaemic strokes [1]. The
most common pattern (75%) on neuroradiological images are
bilateralinfarcts in the territory of paramedian artery or combined
with other thalamic artery theritories. Most of the patient with
bilateral paramedian infarction have specific clinical presentation
with disorder of consciousness, memory dysfunctions, various types
of vertical gaze palsy and psychic changes. The main cause of
bilateral thalamic infarction was small artery-disease, followed by
cardioembolism[1].
CASE REPORT
A 37 year-old woman, previously healthy, during regular
activities on job suddenly became aware of visual disturbances, saw
double pictures and was not able to see left side of the field. She
was alert the whole time, but was complaining of instability,
speaking problems and some kind of transient hearing problem.
Ex-professional basketball player, smoker; without previous illness
and other known risk factors. She strictly denied previous stroke or
any similar problems.
On admission she was alert, orientated, all vital signs were within
normal limits, except slight hypertension. Neurological findings
were skew deviation, without hemianopsia, central facial palsy on
the right side with deviation of tongue to the right, left
hemihypesthaesia, and truncal ataxia. She had no manifest motor
deficit except discrete subjective feeling of weakness of the left
arm. Glasgow Coma Scale (GCS) score was 15, National Institutes of
Health Stroke Scale (NIHSS) score was 7, and Mini Mental Score
Examination (MMSE) was 28. In the next two days she developed
discrete right hemiparesis. Standard laboratory tests, prothrombin
time, partial thromboplastin time, D- dimmer were within normal
limits. An EKG showed normal sinus rhythm.
A computed tomography (CT) with angiography (CTA) of the brain was
normal. Duplex ultrasound imaging of carotid arteries revealed
nonsignificant bilateral stenosis. Transcranial Doppler (TCD) of
vertebrobasilar arteries showed mild hemodynamic changes in right
vertebral artery. TCD of the circle of Willis was normal. Magnetic
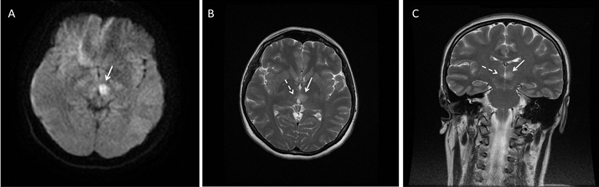
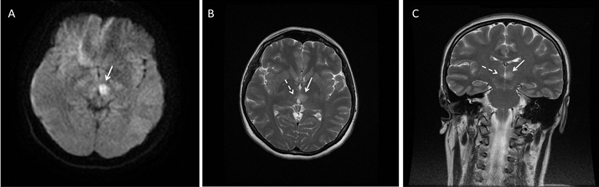
resonance imaging (MRI) of the brain with angiography (MRA) showed
an increase in signal in the thalami bilaterally on T2
fluid-attenuated inversion recovery (FLAIR) sequence with the signs
of restricted diffusion on the left side but without restriction on
the right side suggesting the bilateral thalamic infarction (Fig.1).
Despite the fact that it was not seen on CTA and MRA, the existence
of Percheron’s artery was not excluded. MR venography of the brain
excluded cerebral veins thrombosis.
TCD bubble test was positive and transesophageal echocardiography
(TEE) confirmed patent foramen ovale (PFO). Ultrasound of deep veins
of the legs showed no abnormalities. Further laboratory findings
revealed mild hyperlipoproteinemia, decreased level of folic acid
and borderline elevated homocysteinlevel. Genetic screening revealed
that the patient is homozygous for A1298C mutation in
methylenetetrahydrofolate reductase (MTHFR) gene. Laboratory tests
of vasculitic diseases were negative.
The patient continued to do extremely well while in hospital without
any episodes of alteration in consciousness, with gradually recovery
of symptoms. Neurological findings remained with only slight
diplopia. Mood, behavior and cognition appeared intact with just
minor memory deficit, MMSE 28-29. She was discharged home on
clopidogrel, folic acid and simvastatin therapies 12 days after the
stroke onset. She was recommended for percutaneous closure of PFO
and it was performed six months after the stroke.
At a seven-month follow-up patient report there were no complaints,
no visual disturbances, sensory or motor deficit. Psychological
testing revealed minor memory deficit (MMSE 30).
DISCUSSION
Bilateral thalamic infarctions are rare and associated with
typical clinical patterns [1]. When they occure in the presence of
normal brain and neck CTA, one rare anatomic variant of thalamic
perfusion could be considered - commonly known as the artery of
Percheron, single artery that branches from proximal segment of one
of the posterior cerebral artery and irrigates both paramedian
territories of thalamus [2]. Several short-numbered series and
isolated case reports have been published about bilateral paramedian
thalamic infarcts, but just a few of them associated with PFO [3-6].
Patent foramen ovale occurs in up to 25% of the general population
[7,8]. Several studies about association of PFO with ischaemic
stroke in young people were made and they emphasized the fact that
paradoxical embolism through a patent foramen ovale can be a
possible cause of stroke in young adults [8-10]. Lechat et al found
that PFO occurs in 40% of all young patients with stroke [8]. The
same group of authors also found that in the group with no
identifiable cause (cryptogenic stroke) which included 43 percent of
cases, the most prevalent potential source of cardioembolism was
patent foramen ovale (in 54%). Similar conclusions were obtained in
a study by Webster et al (PFO was found in 50% of the stroke
patients younger than 40 years) [10]. Study by Pezzini et al found a
significant relation between cardioembolism and paramedian infarcts
in young people [10].
Our case is interesting in the context of the combination of the two
specific conditions - paradoxical embolisation and presumed artery
of Percheron. Clinical presentation was not usual for paramedian
thalamic infarcts, the most prominent deficit was visual disturbance
due to skew deviation. There was no consciousness deficit wich is
common for this type of stroke, nor personality or major cognitive
changes. Although MRI of the brain did not show restriction of
diffusion on both paramedian areas, regarding clinical picture that
revealed bilateral neurological deficit and anamnestic data of
visual disturbances at a stroke onset without previous history of
the disease, we are inclined to believe that this was simultaneous
bilateral thalamic infarction.
Figure 1: A) Axial diffusion weighted MRI
shows restriction of diffusion on the left thalamus (white arrow).
B) Axial and C) coronal T2 weighted MRI shows the bilateral
paramedian thalamic infarction, bigger one on the left side (solid
white arrows) and small one on the right (dash white arrows).
REFERENCES
- Kumral E, Evyapan D, Balkir K, Kutluhan S. Bilateral
thalamic infarction. Clinical, etiological and MRI correlates.
Acta Neurol Scand. 2001;103(1):35-42.
- Percheron G. Arteries of the human thalamus. II. Arteries
and paramedian thalamic territory of the communicating basilar
artery. Rev Neurol (Paris). 1976;132(5):309-324.
- Lopez-Serna R, Gonzalez-Carmona P, Lopez-Martinez M.
Bilateral thalamic stroke due to occlusion of the artery of
Percheron in a patient with patent foramen ovale: a case report.
J Med Case Reports 2009;3:7392.
- Chavez-Valencia V, Soto-Cabrera E. Acute bilateral thalamic
infarcts in a young man with patent foramen ovale. Gac Med Mex
2010;146(1):55-58.
- Emond H, Landis T, Perren F. From amaurosis fugax to
asymptomatic bithalamic infarct. J Neurol.
2009;256(6):1007-1008.
- Salam A, Sanmuganathan P, Pycock C. Unusual presentation of
basilar artery stroke secondary to patent foramen ovale: a case
report. J Med Case Reports. 2008;2:75.
- Sacco R.L, Adams R, Albers G, Alberts M.J, Benavente O,
Furie K, et al. Guidelines for prevention of stroke in patients
with ischemic stroke or transient ischemic attack: a statement
for healthcare professionals from the American Heart
Association/American Stroke Association Council on Stroke:
co-sponsored by the Council on Cardiovascular Radiology and
Intervention: the American Academy of Neurology affirms the
value of this guideline. Stroke. 2006;37(2):577-617.
- Thaler D.E, Saver J.L. Cryptogenic stroke and patent foramen
ovale. Curr Opin Cardiol. 2008;23(6):537-544.
- Lechat P, Mas J.L, Lascault G, Loron P, Theard M, Klimczac
M, et al. Prevalence of patent foramen ovale in patients with
stroke. N Engl J Med. 1988;318(18):1148-1152.
- Webster M.W, Chancellor A.M, Smith H.J, Swift D.L, Sharpe
D.N, Bass N.M, et al. Patent foramen ovale in young stroke
patients. Lancet. 1988;2(8601):11-12.
- Pezzini A, Del Zotto E, Archetti S, Albertini A, Gasparotti
R, Magoni M, et al. Thalamic infarcts in young adults:
relationship between clinical-topographic features and
pathogenesis. Eur Neurol. 2002;47(1):30-36.
|
|
|
|