|
||||||||||||||||||||||||||||||||||||
| [ Sadržaj
] [ Indeks autora ]
|
||||||||||||||||||||||||||||||||||||
|
UDK 616.32/.34-005.1-072.1/.2 |
||||||||||||||||||||||||||||||||||||
|
Originalni rad / Original paper Uzrok krvarenja iz gornjih
partija digestivnog trakta i hitna gastroskopija u urgentnom centru
KC Kragujevac Biljana Milojković Kicevska (1), Zoran
Kovačević (1), Mirjana A. Janićijević Petrović (2), |
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Preuzmite rad / Download | Summary:
Introduction: Digestive tract bleeding is a clinical problem that
requires hospitalization. Hemorrhages from the upper parts of the
digestive system have an incidence of 150/100000 persons per year
and are the reason for 1.5% of all emergency hospitalizations. The
most common cause of bleeding is gastroduodenal ulcer and erosion in
three quarters of cases. Endoscopic haemostatic and gastric acidity
status are the most important in the treatment of patients. Aim: To
analyze the causes of bleeding from the upper parts of digestive
tract and the justification for the urgent gastroscopy. The study
was conducted at the Clinical Center Kragujevac in Kragujevac,
Serbia. Methods: The study included patients (200) who reported to
the emergency room of the Emergency Medicine Center with the
clinical picture of bleeding from the upper parts of the digestive
tract. Results: Most patients had ulcerative changes at gastric
level (58.6%). The most common symptom was melena present in 152
patients. Endoscopic therapy was administered to 44 patients, with
38 patients (86.4%) resulting in arresting bleeding. Conclusion:
Hemorrhages from the upper parts of the digestive tract are most
commonly caused by peptic ulcers, more common in older, male
patients. The first form of diagnosis and therapy is endoscopy, with
an efficacy greater than 70%. Keywords: digestive tract, upper parts, bleeding, emergency medicine, endoscopy Sažetak: Uvod: Krvarenje iz digestivnog trakta je klinički problem, koji zahteva hospitalizaciju. Krvarenje iz gornjih partija digestivnog trakta ima incidenciju 150/100000 osoba godišnje i predstavlja razlog 1,5% svih urgentnih hospitalizacija. Najčešći uzrok krvarljenja su gastroduodenalni ulkusi i erozije u tri četvrtine slučajeva. U tretmanu pacijenata najvažniji su endoskopska hemostaza i aciditet želudačnog soka. Cilj: Analiza uzroka krvarenja iz gornjih partija digestivnog trakta i opravdanost urgentne gastroskopije. Istraživanje je sprovedeno u Kliničkom Centru Kragujevca u Kragujevcu, Srbija. Materijal i metode: Istraživanjem su obuhvaćeni pacijenti (200) koji su se u prijemnu ambulantu Centra za urgentnu medicinu javili sa kliničkom slikom krvarenja iz gornjih partija digestivnog trakta. Rezultati: Kod većine pacijenata ulcerozne promene su bile na nivou želuca (58,6%). Najčešći simptom je bila melena prisutna kod 152 pacijenta. Endoskopska terapija je primenjena kod 44 pacijenta, pri čemu je kod 38 pacijenta (86,4%) dovela do zaustavljanja krvarenja. Zaključak: Krvarenja iz gornjih partija digestivnog trakta najčešće su uzrokovana peptičkim ulkusima, češća kod starijih pacijenata, muškog pola. Prvi vid dijagnostike i terapije je endoskopija, sa efikasnošću većom od 70%. Ključne reči: digestivni trakt, gornje partije, krvarenja, urgentna medicina, endoskopija |
|||||||||||||||||||||||||||||||||||
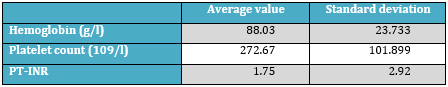
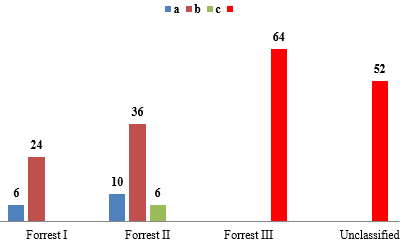
INTRODUCTIONGastrointestinal bleeding is defined by the appearance of blood in the digestive tube. The clinical manifestation of bleeding depends on the site of bleeding, the severity of bleeding, and the existence of co-morbidities, and it is divided into bleeding from the upper (90%) and bleeding from the lower intestinal tract (10%) [1, 2, 3]. In the case of a hemodynamic unstable patient, the measures that are applied are the hemodynamic restitution with infusion solution, oxygen therapy, and reimbursement of blood derivatives, with constant monitoring of vital parameters. Emergency esophagogastroscopy is the method of choice and is conducted according to the protocol in the first 12-24 hours [4]. Endoscopic examinations, as a special type of examinations, or within fiber pan-endoscopy, are carried out for diagnostic and interventional purposes (operative-therapeutic) [4]. The most common indications for diagnostic and therapeutic endoscopy of the upper gastrointestinal tract are: pyrosis or persistent pain despite medication therapy, dysphagia, odynophagia, the evaluation of the symptoms of hematemesis or hidden bleeding after surgery, the evaluation of abnormal contrast radiography, biopsy of gastric ulcers and neo-plastic lesions [4, 5]. Specific indications are foreign body extraction and assessment of the degree of mucosal lesions after the caustic ingestion and the control of pre-malignant conditions, Barrett's esophagus and gastric polyps [5, 6, 7]. Contraindications are: acute respiratory and cardiovascular insufficiency; coma and delirium types of different origin; acute corrosive changes in the esophagus; indiscipline and lack of cooperation of the patient during the examination. Eight hours prior to the intervention the patient must not take anything by mouth, except in emergencies, if acute bleeding in the upper parts of the digestive tube occurs, in which case immediately after the arrival and hospitalization, the nasogastric tube is placed into the patient; this not only has the diagnostic role, but also a role in preparing a patient for urgent esophagogastroduodenoscopy as well [8]. Esophagogastroduodenoscopy allows inspection of the upper segment of the gastrointestinal tract, thus called upper pan-endoscopy. Endoscopic examination analyzes lumen, motility, the appearance of mucosa, and taking biopsy of cytological samples or aspirates from the lumen [9]. Esophageal and cardiac cancers are endoscopic observed, as well as the changes such as plaque, nodular thickening or ulcerative lesions. Gastric lesions which are endoscopic identified: congenital abnormalities, vascular malformations, postoperative mucosal changes, foreign bodies, hiatus hernia, pyloric stenosis which is observed due to pyloric hypertrophy or inflammation. Gastric inflammatory lesions are common findings on the endoscopy and include various forms: gastritis, fresh ulceration or infiltrative process, such as an eosinophilic granuloma. Vascular lesions: gastric varices, arteriovenous gastric ectasia, angiodysplasia and "watermelon stomach" are identified as bleeding sites [10]. Of all the sources of bleeding from the upper intestine, one third accounts for the esophagus (36%), the varicose veins of the esophagus, then Mallory-Weiss syndrome, esophageal cancer, and esophagitis. Another third (about 37%) belongs to the sources from the stomach, where the most common are ulcer and erosive gastritis, and less often gastric cancer. The remaining 27% of cases of bleeding belong to the duodenum, where the most common is ulcer, the rare diverticular bleeding, or the bleeding from multiple duodenal erosions [11]. MATERIAL AND METHODSThe study was conducted at the Clinical Center Kragujevac, by combining retrospective and prospective research methodology. The study included 200 patients, who were reported to the outpatients’ department of the Center for Emergency Medicine of the Clinical Center with clinical signs of bleeding from the upper parts of the digestive tract (hematemesis, melena). Patients were presented with their rights and obligations that they assumed for participating in the study, as well as the potential risks and disadvantages of the study. In addition to the detailed anamnesis and an initial examination, complete laboratory analysis, emergency and contol esophago-gastroduodenoscopy and echosonography of the abdomen were performed for each patient. Apart from determining the clinical and laboratory parameters, specific demographic data of patients were collected: age, sex, profession, place of residence, associated disease and intake of medication, as well as information about any possible episodes of previous bleeding from the gastrointestinal tract. The patients of both sexes, aged 16 to 80 years, were included. Including criteria was: the patients with symptoms of bleeding of the upper parts of the digestive tract (hematemesis, melena) and the patients who had signed a voluntary consent for the endoscopic procedure. Excluding criteria was: the patients under 16, pregnant or lactating women, the patients with malignancies on cytostatic therapy, the patients with other life-threatening conditions and the ones who refused endoscopy. The study used the "convenience" sample (subjects that met criteria were included in succession). The information on basic patients’ characteristics were analyzed and presented using descriptive statistics method. For continuous variables, the mean values ± standard deviation were used, minimum and maximum, if the data followed a normal distribution, or the median and percentiles if the data did not follow a normal distribution, while the frequency (percentages) was used for categorical variables. All the data were analyzed using the IBM statistics SPSS version 21 software. RESULTSThe distribution of patients by gender was 40% of females and 60% of males. The average age of patients was 68.64 years with a standard deviation of 14.3 years. The oldest patient was 94 years old, the youngest 25 years old. Based on the average age of the patients (68.64 ± 14.3) these were elderly patients. Out of the 200 patients, 92 patients (46.5%) had hematemesis, 152 patients (76.8%) had melena, while 46 patients (23.2%) had both symptoms. The average value and standard deviation value of hemoglobin, platelet count, INR (international normalized ratio of prothrombin time) are shown in Table 1. Table 1. The average value and standard deviation
value of hemoglobin, The average time elapsed from the first
esophago-gastroduodenoscopy in the study participants was 6.5 hours.
In 54 patients (27.3%), the presence of acute bleeding was revealed
by endoscopy, in 10 patients (5.1%) the existence of Mallory-Weiss
syndrome, in 46 patients (23.2%) the existence of erosive changes.
In the majority of the patients 164 (82.8%), the presence of
ulcerative changes of different localization and the degree of
damage was found. Graph 1. The Forrest classification of endoscopic
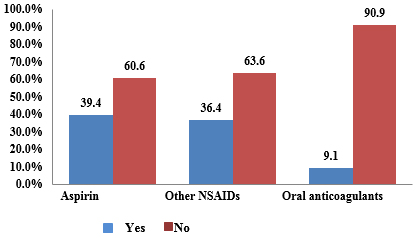
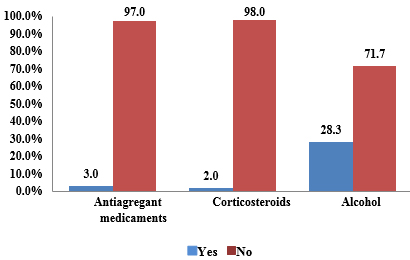
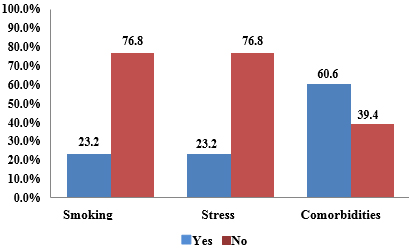
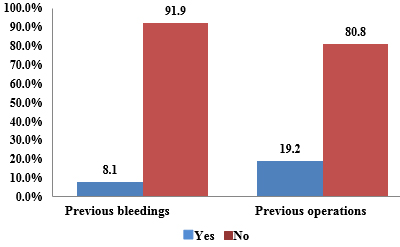
observed bleeding The localization of identified ulcerative changes on the esophagus were 22 (11.1%), stomach 116 (58.6%) and duodenum 32 (16.3). In 60 patients with an ulcerative change at the level of the stomach, the change was located in the gastric antrum, which is 52% of all gastric ulcers. The infiltrates in histological "bioptate" preparations collected during endoscopies, were observed in 16 patients (8.1%). Only 6 patients (3%) had polypoid changes. Endoscopic treatment was performed in 44 patients (22.2%), whereby the various forms of this treatment were applied evenly, such as the usage of adrenaline locally, the placement of mechanical hemo-clips or a combination of previous two. In 38 patients (86.4%) endoscopic treatment was successful, while in 6 patients (13.6%) a surgical intervention was required. After endoscopic examination it was determined that in 14 patients there was an immediate need for surgical intervention. In 20 patients (10.1%) the issue was about re-bleeding, which meant that in their medical histories there were records of previous gastrointestinal bleeding. The exposure to factors associated with the occurrence of bleeding in the gastrointestinal tract is shown in the Graphs 2, 3, 4, 5. Graph 2. The exposure to factors associated with
the occurrence of bleeding in gastrointestinal tract Graph 3.The exposure to factors associated with
the occurrence of bleeding in the gastrointestinal tract Taking all comorbidities into account, hypertension is the most common - 30.4% of all participants in the study, or 50% of all the patients with some of the co-morbidities. Risk factors: aspirin (39.4%), other non-steroidal anti-inflammatory medicaments (36.4%), smoking and stress in (23.2%) of patients. DISCUSSIONBleeding from the digestive tract is a serious clinical problem
which in most cases requires hospitalization. Due to the dramatic
clinical picture and requirements for urgent therapeutic and
diagnostic procedures, acute gastrointestinal bleedings are among
the high priorities of pre-hospital and hospital treatments. The
patients with a single episode of ulcer bleeding have twice the risk
of new bleeding in their lifetime, while the patients with two
episodes of bleeding have more than 35% chance of re-bleeding [12].
In the treatment of these patients, the most important are
endoscopic haemostasis in order to avoid unnecessary surgery, and
medicaments that reduce the acidity of the gastric juice (proton
pump inhibitors). Between 3% and 15% of bleeding episodes are
treated surgically [13]. Risk factors are mainly related to
socio-demographic characteristics of the patients and their life
habits, but risk factors are also represented by a certain group of
medicaments. Oral anticoagulants, antithrombotics, corticosteroids
and non-steroidal anti-inflammatory medicaments are distinguished as
the most important groups. Non-steroidal anti-inflammatory drugs
have significant potential for the provocation of bleeding of the
upper parts of the digestive system and taking this parameter into
account, the drugs from the group of selective inhibitors of
cyclooxygenase2 [13, 14] are significantly safer. The most dangerous
bleeding from the digestive tract may be caused by oral
anticoagulants, in cases of inadequate adjustments of their doses
according to the value of INR. Bleeding from the upper parts of the
digestive system caused by the action of oral anticoagulants
requires urgent endoscopy. The first step in the treatment of all
the patients with bleeding from the digestive tract is a rapid
assessment of the severity of bleeding, immediately followed by the
measures of liquid volume reimbursement which include an initial
fluid administration through wide intravenous lines [13, 14]. With
bleeding from the upper parts of the digestive system under
conditions of the highest quality of treatment, progress in the
diagnostics and non-surgical methods of haemostasis, technological
advances in the field of intensive care, mortality rate is 7-10% and
has not changed for the last forty years [14, 15]. The level of
mortality because of the bleeding from the upper parts of the
digestive system requires urgent diagnostic and therapy [15].
Duodenal ulcers are definitely the leading cause of bleeding from
the upper parts of the digestive tract [16]. Two traditional types
of endoscopic therapy are the adrenaline therapy and the clip-based
therapy [17, 18]. Esophago-gastroduodenoscopy is an efficient method
for the diagnosis and treatment of the patients with bleeding from
the upper parts of digestive tract [19]. In our study,
esophago-gastroduodenoscopy was administered relatively quickly,
with an average time of 6.5 hours from the beginning of bleeding.
The world generally accepts the trend that endoscopy is the first
line of treatment to stop the bleeding from the upper parts of the
gastrointestinal tract. Endoscopic methods are often supplemented by
using the anti-secretory therapy, although there are experts who
believe that the administration of erythromycin as a prokinetic may
have a positive influence on hemostasis from the gastrointestinal
tract [20]. Contemporary guides advise the use of proton pump
inhibitors and erythromycin, as adjuvant therapy for endoscopy with
the purpose of hemostasis [21]. In spite of the high efficiency and
effectiveness, endoscopic methods are still not able to reduce
mortality caused by the digestive tract bleeding [22]. Despite the
fact that several new endoscopic methods are presently still in the
experimental phase [22, 23] and that the current results indicate
that these methods are more efficient than existing endoscopic
methods, it is important to emphasize that even these advanced
endoscopic techniques are not followed by a reduction in mortality.
The most important advantage of new endoscopic methods compared to
conventional ones, in addition to undoubtedly higher efficiency, is
the lower rate of complications, since the endoscopy is often known
to be accompanied by the appearance of perforations and iatrogenic
bleeding [23]. When referring to the certainty that endoscopic
methods do not reduce mortality in patients with bleeding from the
upper part of the digestive tract, it is important to note that in
these patients death occurs not as a result of unsuccessful
endoscopic therapy, but mainly because of the characteristics of
these patients: elderly patients usually die due to the inability of
the body to cope with the problems associated with the blood loss
due to bleeding [24, 25]. When it comes to the implementation of
pharmaco-economic aspects of endoscopy as a therapeutic option to
stop the bleeding from the digestive system, the results of study
that was carried out are in favor of the fact that endoscopy is a
cost-effective therapeutic measure. Endoscopy is much more
cost-effective than surgical operations. Surgery should be
undertaken when endoscopy does not lead to the expected results. It
has been shown that, from the pharmaco-economic point of view, a
combination of the endoscopic methods with proton pump inhibitors
can be considered to be cost-effective [26]. CONCLUSIONThe most common cause of bleeding is gastroduodenal ulcer and erosion in three quarters of cases. and the most common symptom was melena present in 152 patients. Hemorrhages from the upper parts of the digestive tract are most commonly caused by peptic ulcers, more common in older, male patients. Risk factors are associated with the occurrence of bleeding in gastrointestinal tract mainly related to socio-demographic characteristics of the patients and their life habits, but risk factors are also represented by a certain group of medicaments. Oral anticoagulants, antithrombotics, corticosteroids and non-steroidal anti-inflammatory medicaments are distinguished as the most important groups. The first form of diagnosis and therapy is endoscopy, with an efficacy greater than 70%. Endoscopic therapy was administered to 44 patients, with 38 patients (86.4%) resulting in arresting bleeding. Two traditional types of endoscopic therapy are the adrenaline therapy and the clip-based therapy. Conflict of interest: The authors report no conflict of interest. REFERENCES:
|
||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||
| Adresa autora / Corresponding
address: Biljana Milojković Kicevska, Department of Internal medicine, Clinical Centre of Kragujevac, Kragujevac, Serbia E-mail: draganki1@msn.com |
Rad primljen: 17.10.2019 Elektronska verzija objavljena: 25.2.2020 |
|||||||||||||||||||||||||||||||||||
| [ Sadržaj
] [ Indeks autora ]
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||